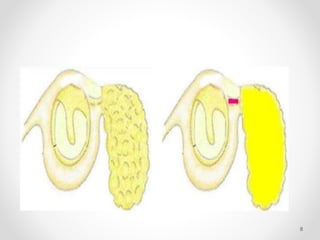
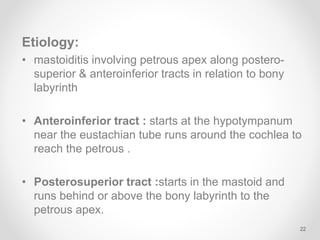
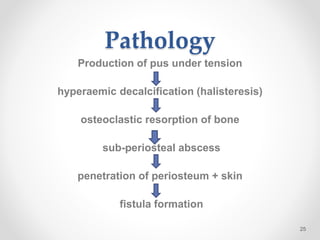
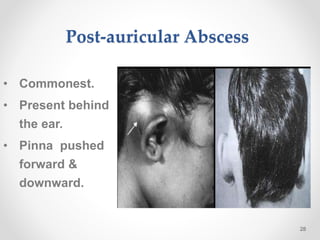
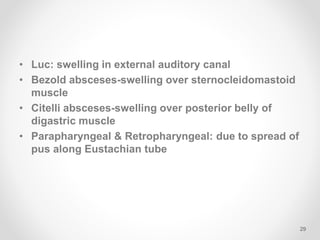
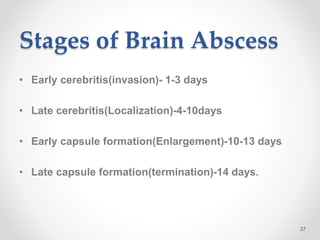
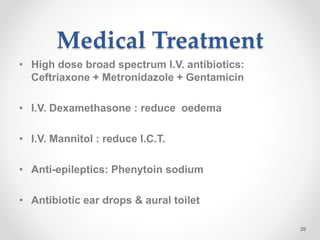
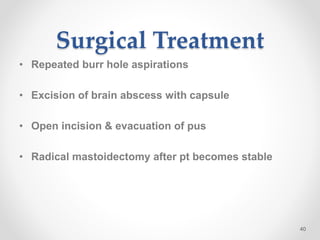
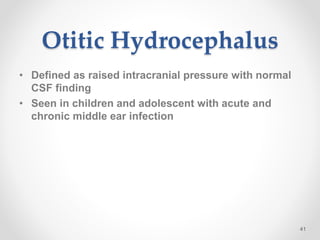
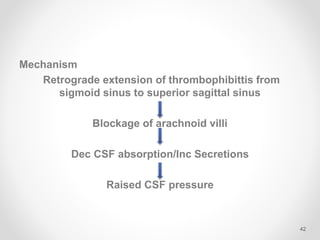
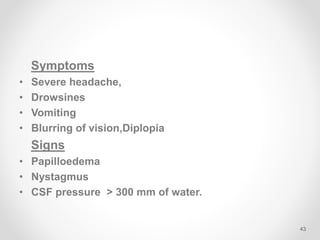
This document discusses various complications that can arise from chronic suppurative otitis media (CSOM). It classifies complications as either intracranial or extracranial/intratemporal. Some potential complications described include mastoiditis, facial nerve paralysis, labyrinthitis, petrositis, subperiosteal abscesses, meningitis, brain abscesses, otitic hydrocephalus, extradural abscesses, subdural abscesses, and lateral sinus thrombosis. Factors that influence the risk of these complications include pathogen virulence, patient immune status, and anatomical defects.