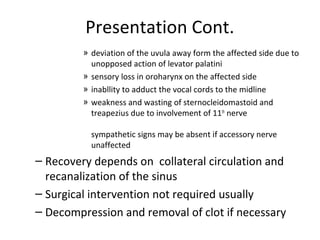
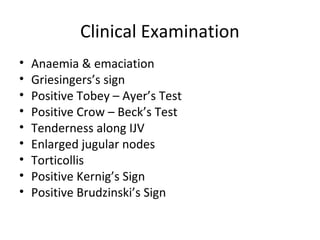
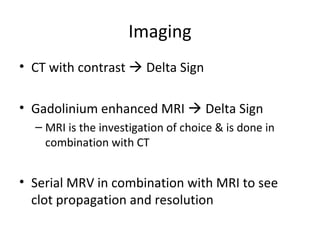
Lateral sinus thrombosis is a complication of chronic suppurative otitis media (CSOM) where infection spreads from the middle ear to the lateral sinus through bone erosion or thrombophlebitis of emissary veins. It can cause symptoms like fever, headache, and neurological deficits depending on the stage of infection. Diagnosis is made through imaging modalities like CT and MRI scans. Treatment involves long-term intravenous antibiotics and possible surgical drainage of infection and removal of blood clots from the sinus. Even with treatment, lateral sinus thrombosis carries risks of complications and death in some cases.