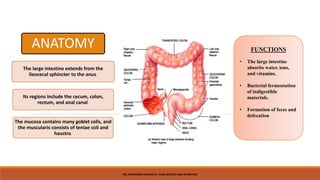
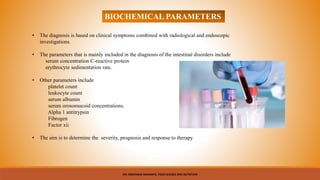
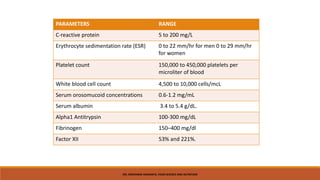
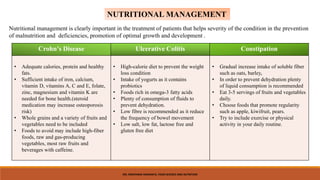
The document discusses the anatomy, functions, digestion and role of bacteria in the large intestine. It also summarizes ulcerative colitis, Crohn's disease and constipation by comparing their symptoms, diagnosis, causes and common treatments. Key biochemical parameters for diagnosing intestinal disorders are outlined. The importance of nutritional management for conditions like Crohn's disease, ulcerative colitis and constipation is highlighted. A case study treatment plan for Crohn's disease focuses on achieving goals like weight gain, normalizing stool and managing gastrointestinal complaints through an enriched diet and supplementation.