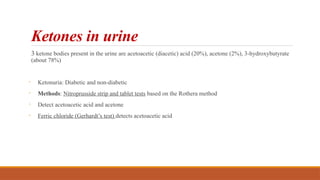
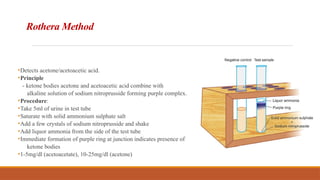
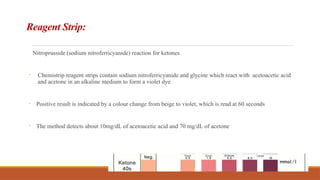
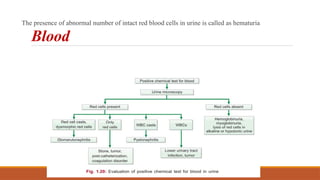
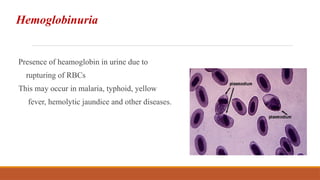
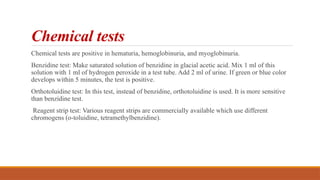
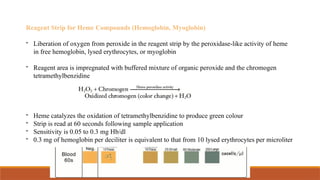
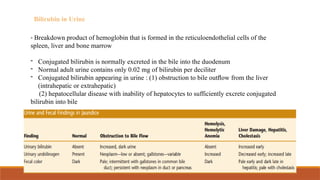
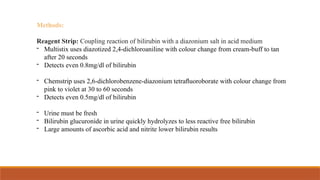
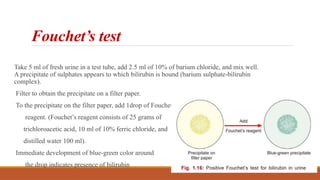
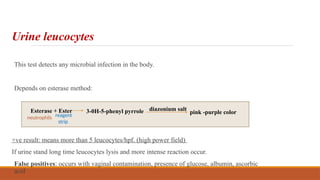
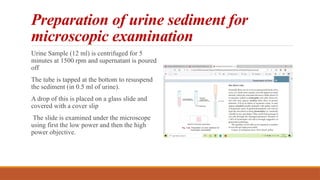
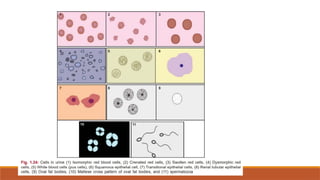
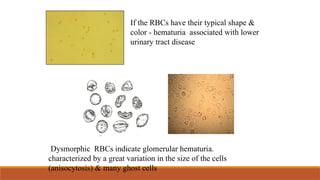
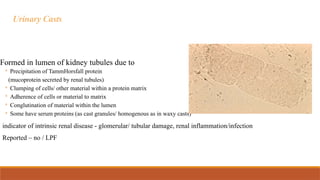
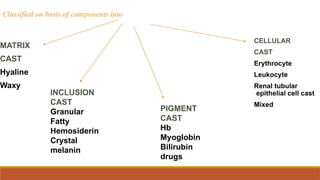
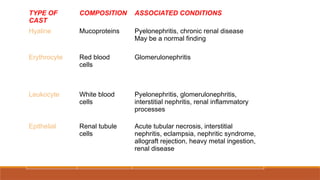
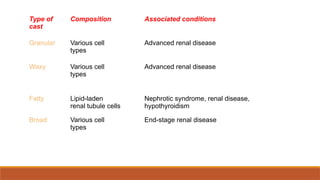
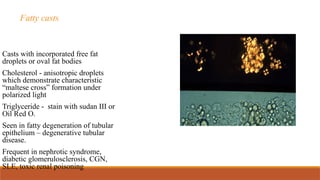
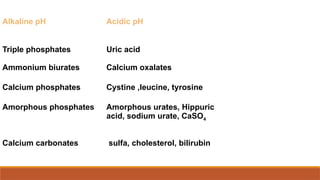
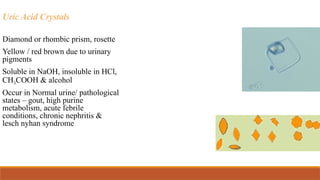
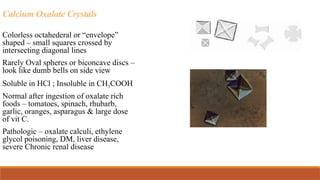
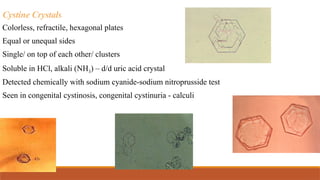
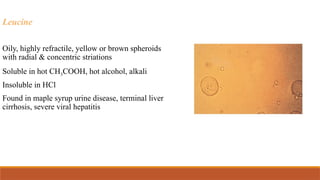
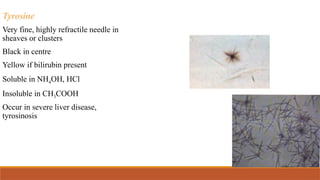
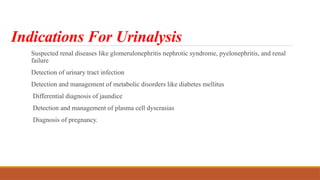
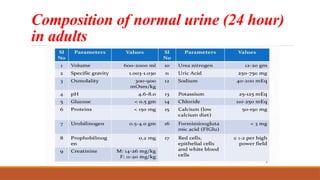
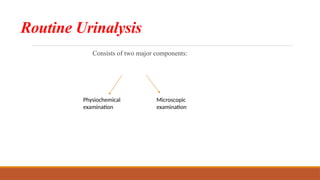
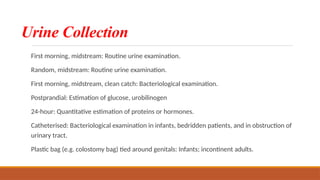
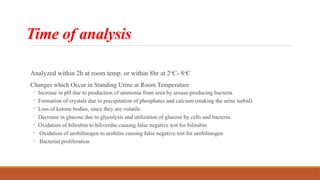
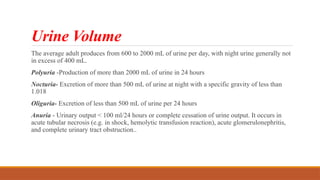
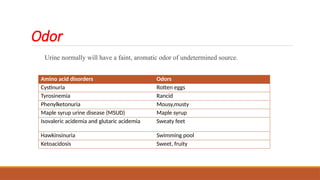
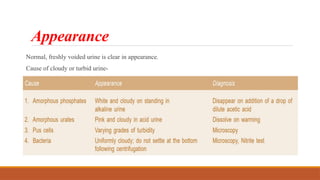
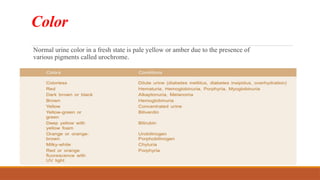
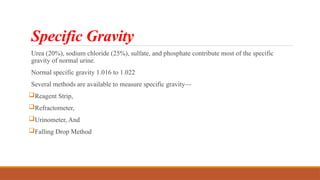
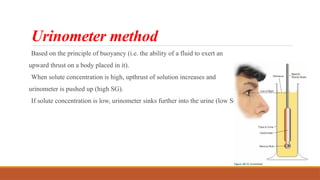
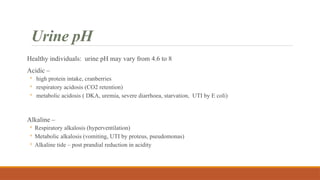
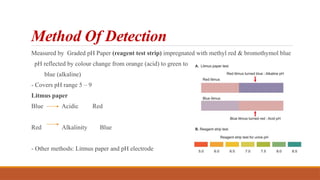
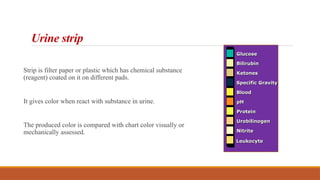
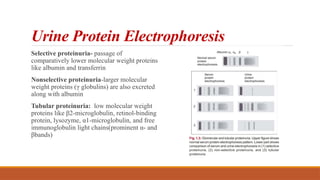
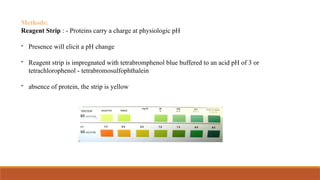
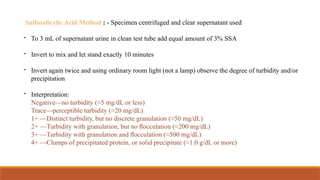
The document outlines the indications and methods for urinalysis, covering the examination of suspected renal diseases, urinary tract infections, and metabolic disorders. It describes urine composition, collection techniques, physical and chemical examination methods, and specific tests for substances like proteins, glucose, and ketones. The document also discusses interpretation of results and various methods for detecting abnormalities in urine.



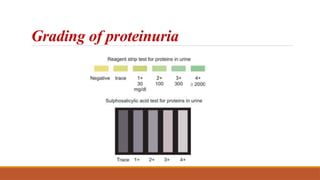
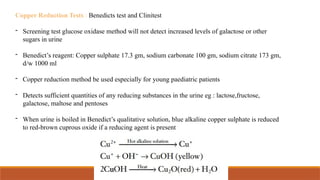
![Interpretation
Blue solution – Negative
Green colour - Traces [<0.5gm/dL]
Green brown - + [0.5 - 1%]
yellow ppt - ++ [1 – 1.5%]
Orange ppt - +++ [1.5 - 2%]
Brick red ppt - ++++ [>2.0gm/dL]](https://image.slidesharecdn.com/urineexamination-250202104245-a6b2a9b8/85/URINE-EXAMINATION-and-its-analysis-presentation-pptx-32-320.jpg)