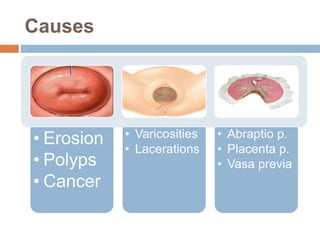
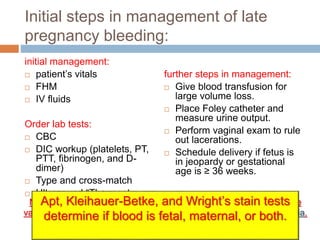
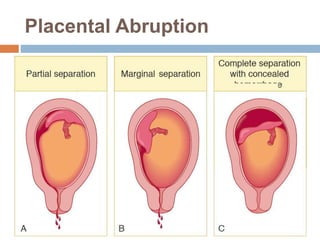
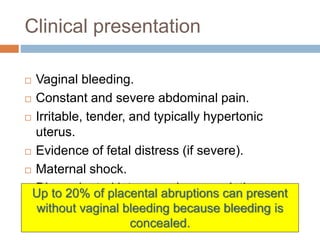
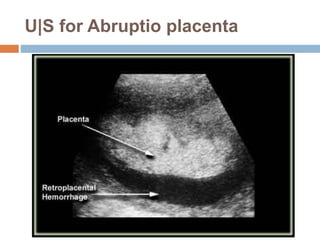
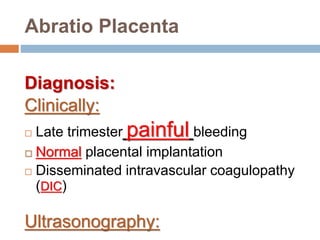
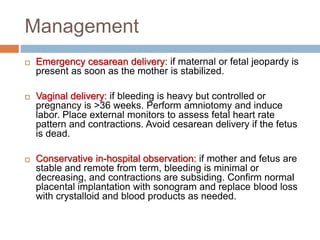
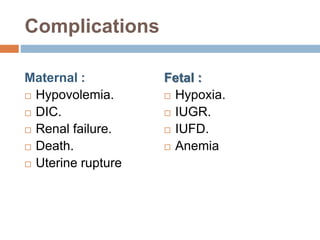
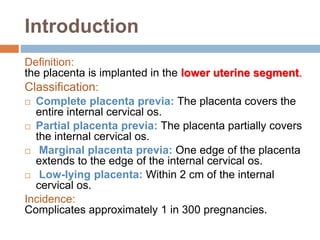
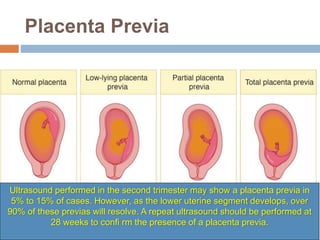
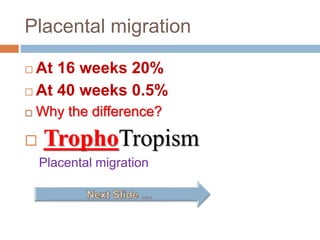
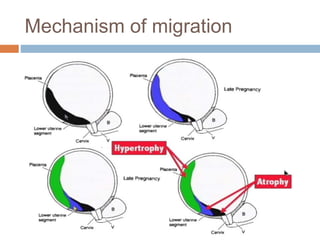
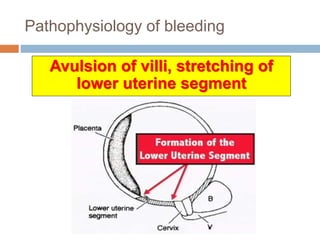
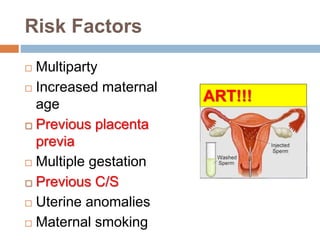
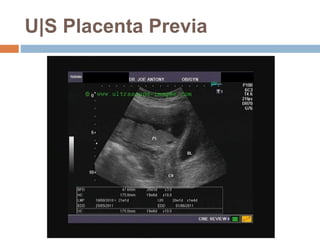
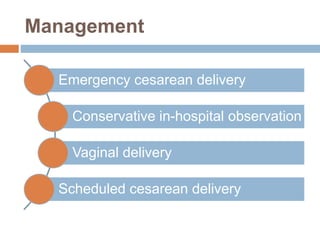
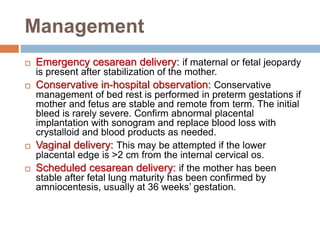
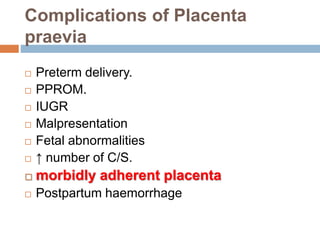
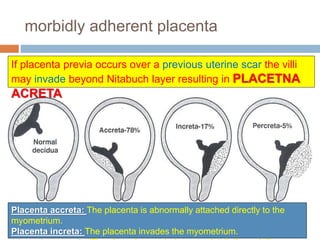
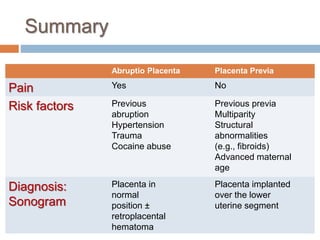
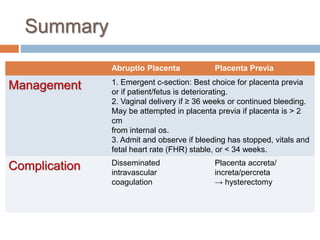
The document discusses two conditions that can cause bleeding in late pregnancy - abruptio placenta and placenta previa. Abruptio placenta involves the separation of the placenta from the uterus prior to delivery and common risk factors include hypertension and trauma. Placenta previa occurs when the placenta implants in the lower uterine segment over the cervical os. Management of both conditions involves monitoring for maternal and fetal stability and either emergency c-section or planned c-section depending on gestational age and severity of bleeding. Complications can include disseminated intravascular coagulation for abruptio placenta or placenta accreta if placenta previa occurs over a previous c-section