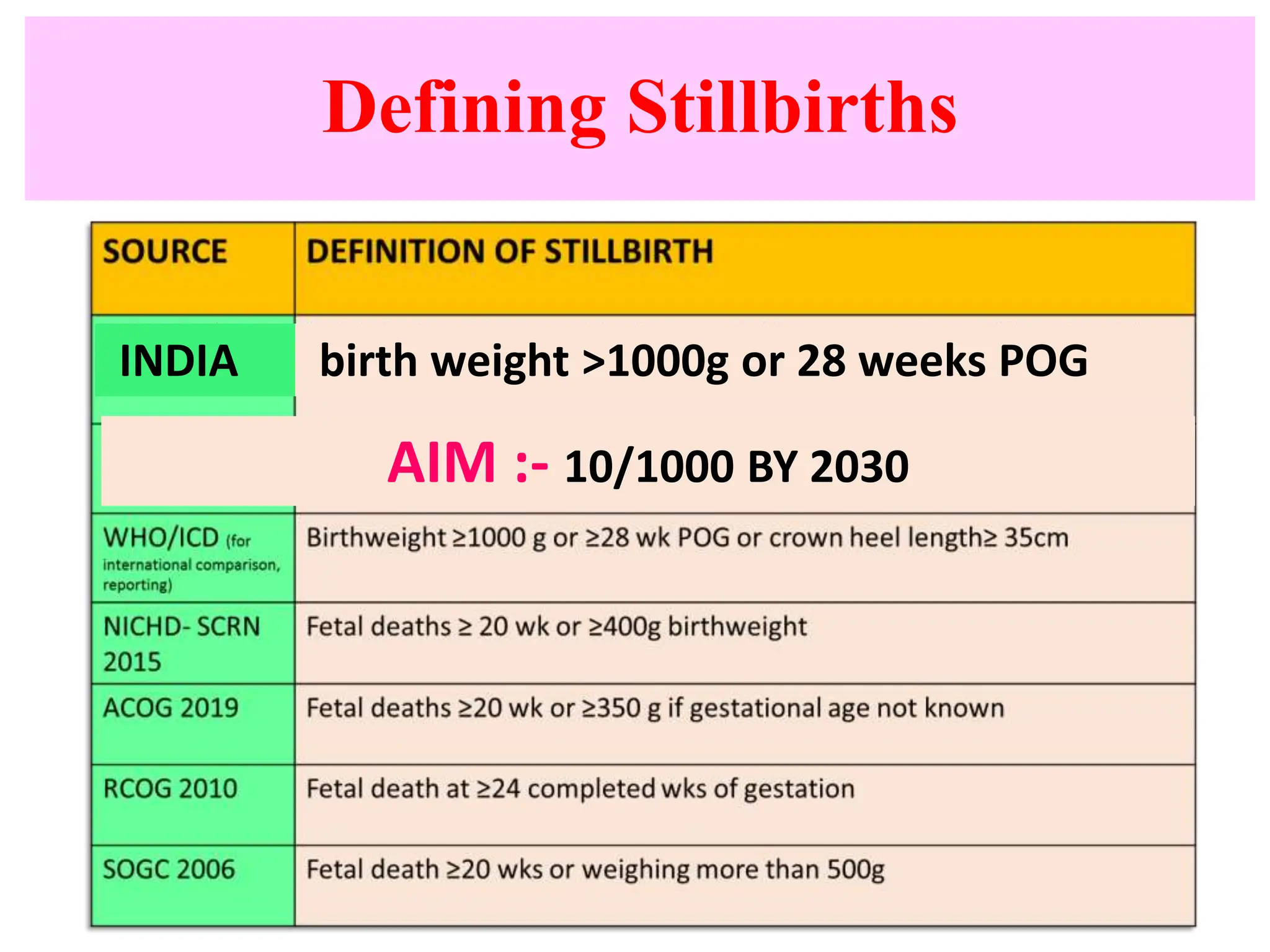
This document provides an overview of stillbirths including definitions, epidemiology, etiology, approaches to management of stillbirth cases and subsequent pregnancies. It notes that the stillbirth rate in India in 2021 was 12.4 per 1000 births. Investigating the causes of stillbirth involves examining the mother, fetus, placenta and membranes through history, examinations, tests and potentially an autopsy. Managing subsequent pregnancies after a stillbirth includes increased surveillance and optimizing any medical conditions to reduce recurrence risks. The aim is to reduce India's stillbirth rate to 10 per 1000 births by 2030.