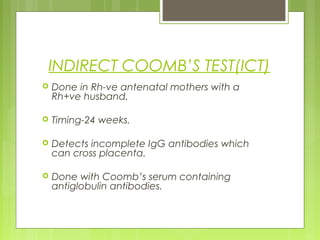
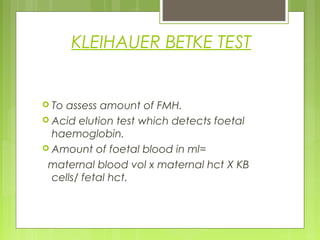
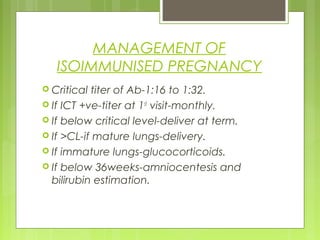
Rh negative pregnancies can lead to isoimmunization of the mother if she has a Rh positive baby. This occurs due to a fetomaternal hemorrhage which allows the fetus's Rh positive blood cells to enter the mother's circulation and trigger an immune response. Testing for isoimmunization involves indirect Coombs testing of the mother. Unsensitized Rh negative mothers receive anti-D immunoglobulin injections to prevent isoimmunization. Sensitized pregnancies require careful monitoring and may involve amniocentesis, intrauterine transfusions or early delivery to prevent fetal complications like hydrops fetalis. The baby may also require treatments like phototherapy or exchange transfusion if affected by hemolytic anemia or