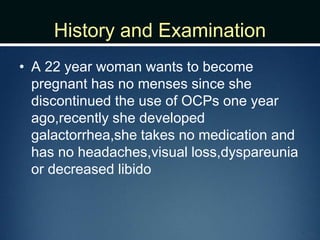
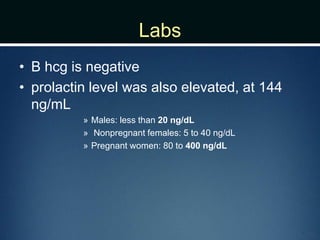
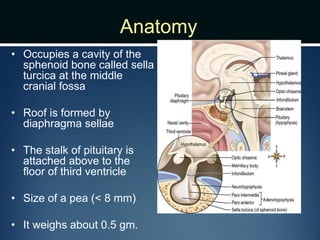
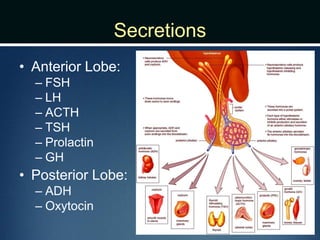
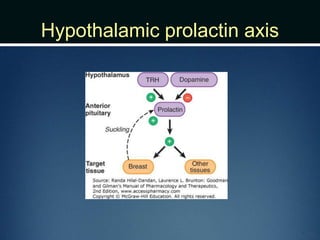
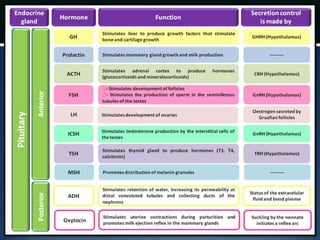
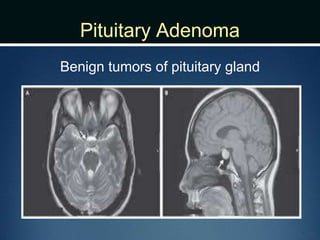
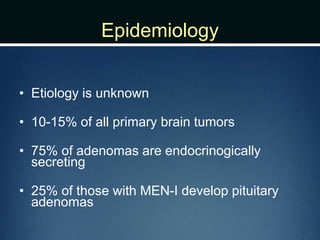
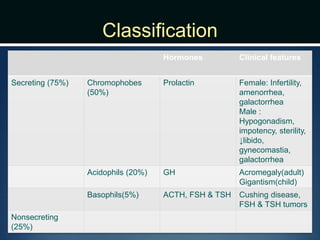
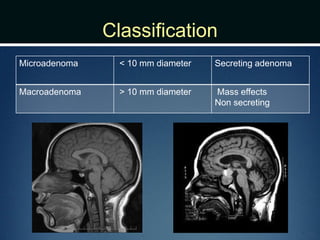
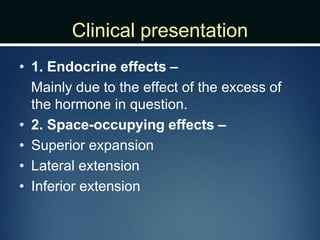
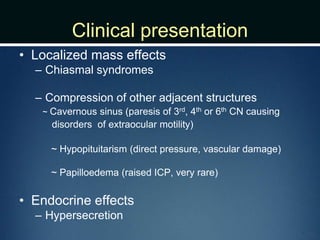
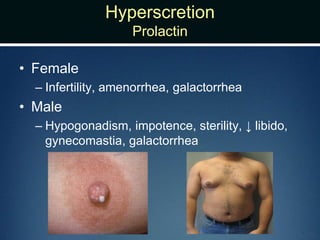
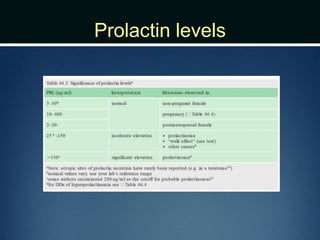
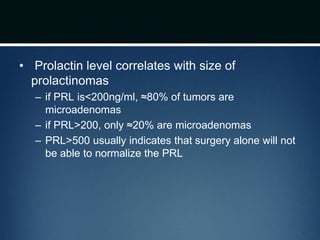
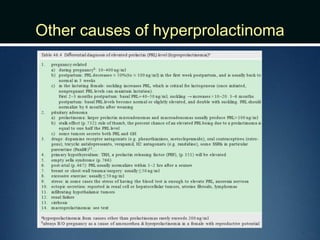
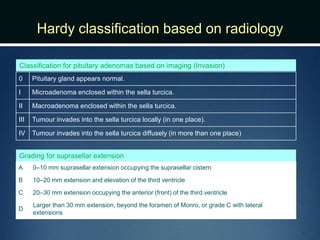
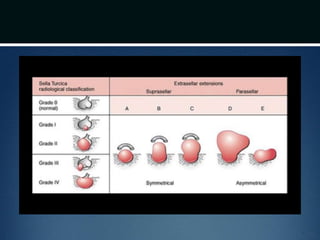
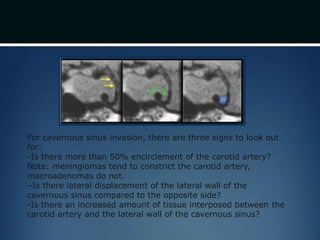
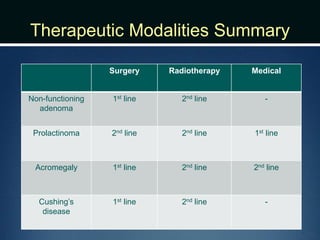
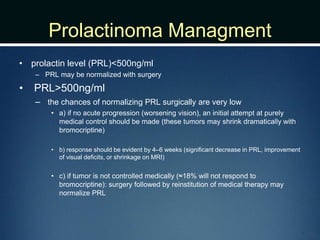
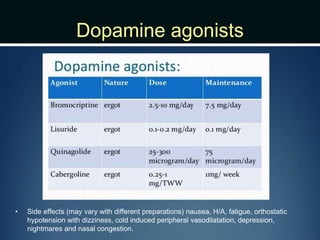
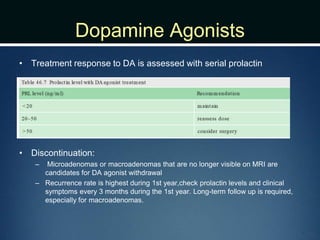
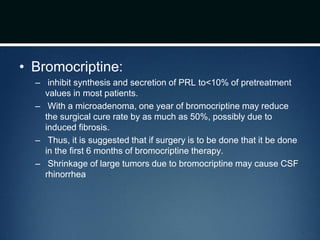
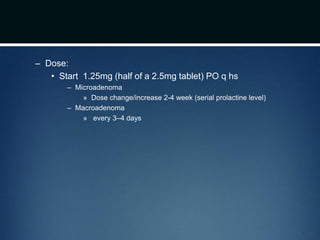
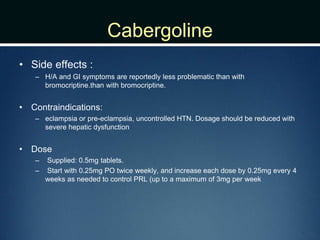
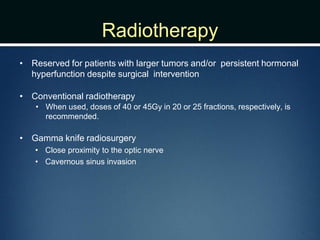
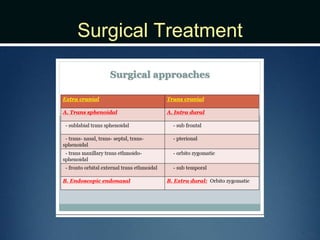
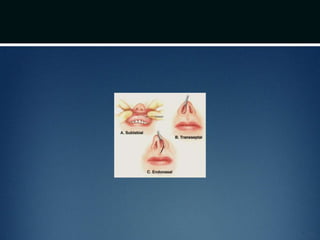
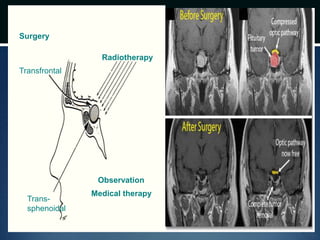
This case involves a 22-year-old woman presenting with galactorrhea and amenorrhea. Her prolactin level was elevated at 144 ng/mL. MRI showed a 5mm microadenoma in her right pituitary gland. She was prescribed cabergoline to lower her prolactin levels, with plans to follow up in 2-3 months. The document then provides background information on pituitary adenomas including causes, classifications, clinical presentations, investigations and management options such as surgery, medication and radiotherapy. The main treatment discussed is dopamine agonists as first-line therapy for prolactinomas.