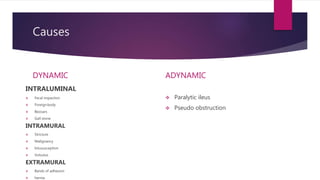
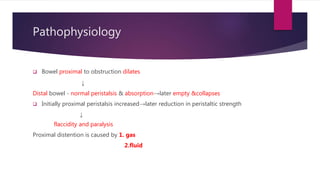
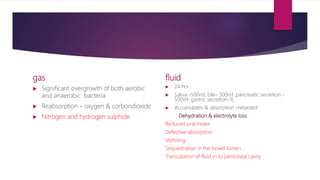
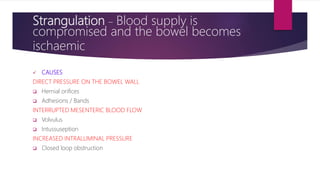
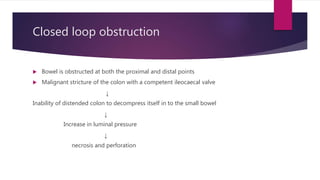
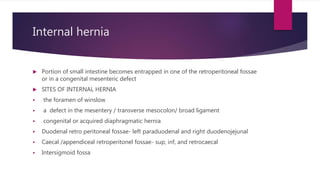
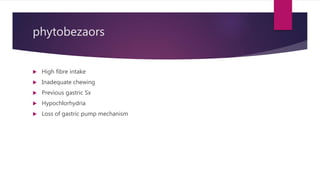
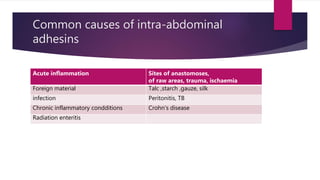
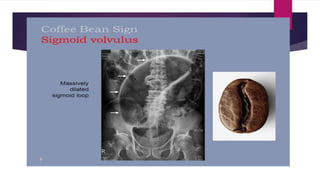
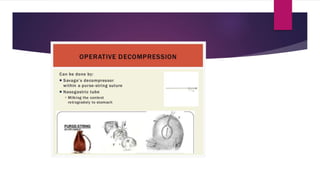
Intestinal obstruction can be classified as dynamic or adynamic. Dynamic obstruction occurs when peristalsis works against a mechanical obstruction, while adynamic obstruction features no mechanical obstruction and lack of peristalsis. Causes include intraluminal, intramural, or extramural factors. Pathophysiology involves dilation of bowel proximal to obstruction and later fluid accumulation. Investigations include abdominal x-rays and CT scans. Treatment involves supportive care like NPO and IV fluids as well as surgical interventions like laparotomy, adhesiolysis, and resection depending on the specific cause and viability of the bowel.