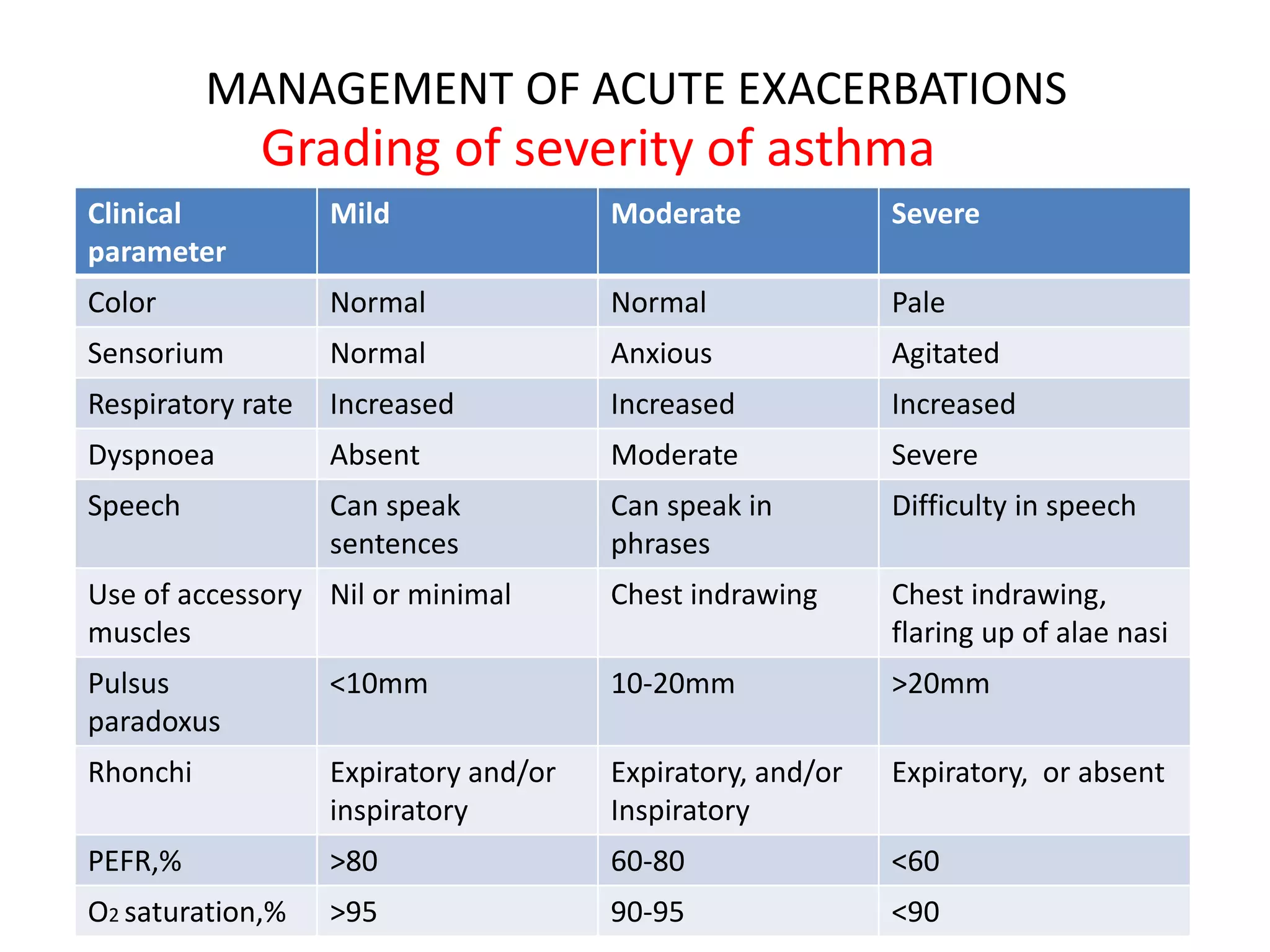
This document provides information on the management of acute exacerbations of asthma. It defines an exacerbation as an increase in cough, wheeze and breathlessness. Exacerbations are classified as mild, moderate or severe/life-threatening based on symptoms and measurements like peak expiratory flow rate (PEFR). For mild exacerbations, short-acting beta agonists are recommended. For moderate/severe exacerbations, additional treatments like oral corticosteroids and oxygen are used. Life-threatening exacerbations require emergency treatments including supplemental oxygen, nebulized bronchodilators and injectable medications, and patients may require intensive care or ventilation if symptoms do not improve. Clinical signs, response to treatment and measurements are used to