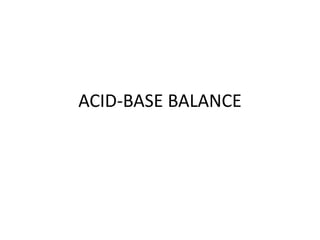
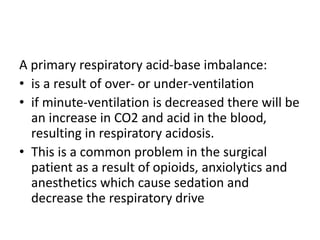
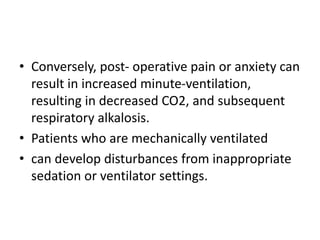
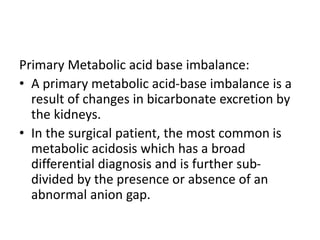
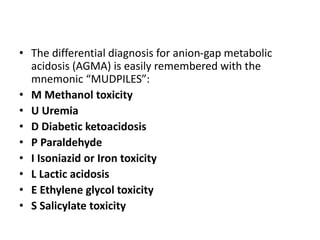
The document discusses acid-base balance and disturbances. It defines the two main buffer systems - metabolic (kidneys) and respiratory (lungs) - that work to maintain blood pH between 7.35-7.45. Five primary acid-base imbalances are described: metabolic acidosis, metabolic alkalosis, respiratory acidosis, respiratory alkalosis, and mixed disturbances. Diagnosis involves blood tests including arterial blood gases and electrolytes to classify the disturbance based on pH, PCO2, and bicarbonate levels. Treatment focuses on addressing the underlying cause rather than just the pH effect.
![Introduction to Acid –Base balance
• The hydrogen ion concentration of body fluids is
maintained within a narrow range for purposes of
regulating normal metabolic and enzymatic
processes and critical functions such as
fertilization, growth, cell volume regulation, and
protein synthesis.
• Since the [H + ] is in nanomolar concentrations,
compared to bicarbonate in millimolar amounts, it
is clear that the [H + ] is involved in many
reactions.](https://image.slidesharecdn.com/acid-basebalance-230924090200-96ebf9c9/85/ACID-BASE-BALANCE-pptx-2-320.jpg)
![Suggested method to approach diagnosis of
acid-base pathology:
1. “emia” - Check the arterial pH
a. pH < 7.4 = Acidemia
b. pH > 7.4 = Alkalemia
2. osis” - Look at the pattern in PCO2 & [HCO3]
• If both PCO2 & [HCO3] are low
Suggests presence of metabolic acidosis or
respiratory alkalosis](https://image.slidesharecdn.com/acid-basebalance-230924090200-96ebf9c9/85/ACID-BASE-BALANCE-pptx-16-320.jpg)
![• If both PCO2 & [HCO3] are high
Suggests presents of metabolic alkalosis or
respiratory acidosis
• If PCO2 & [HCO3] move in opposite directions
Mixed disturbance
• If high anion gap is present
Strongly suggests metabolic acidosis
• If there is a base deficit**
Metabolic acidosis
Can also be a result of compensation](https://image.slidesharecdn.com/acid-basebalance-230924090200-96ebf9c9/85/ACID-BASE-BALANCE-pptx-17-320.jpg)