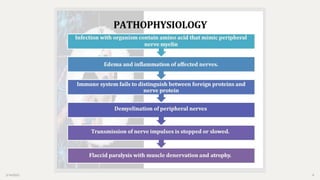
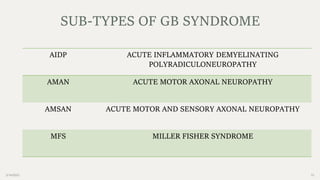
Guillain-Barré syndrome is a rare disorder where the immune system attacks the peripheral nervous system, causing muscle weakness and paralysis. It is usually preceded by a bacterial or viral infection. The main types are acute inflammatory demyelinating polyneuropathy, acute motor axonal neuropathy, and Miller Fisher syndrome. Clinical features include ascending paralysis and respiratory failure. Investigations include lumbar puncture, nerve conduction studies, and antibody testing. Treatment involves supportive care, plasmapheresis, IV immunoglobulins, and most patients recover fully, though some have persistent disability. Homeopathy treatments include Conium, Causticum, Lathyrus, and Natrum Mur depending on symptoms.