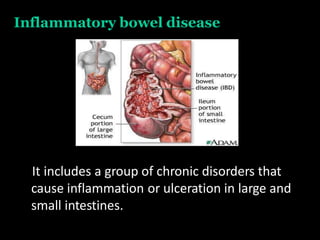
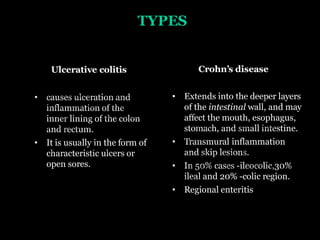
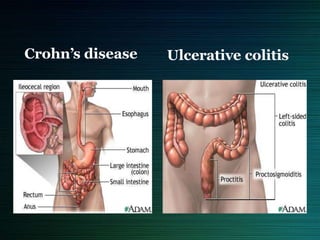
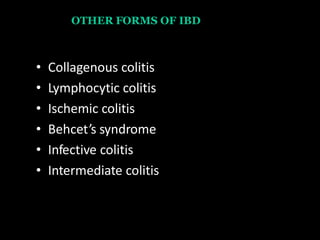
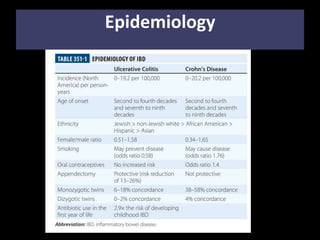
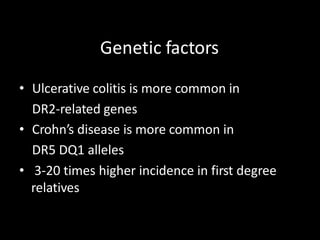
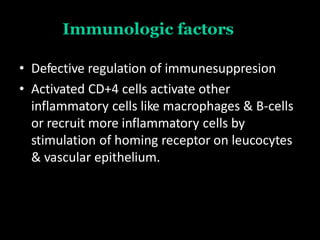
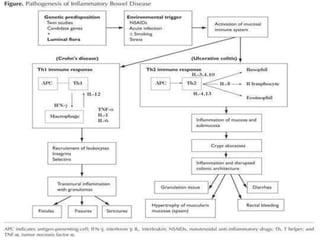
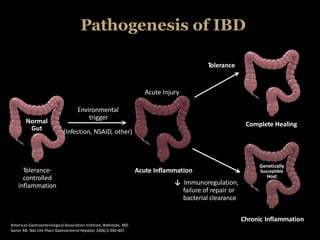
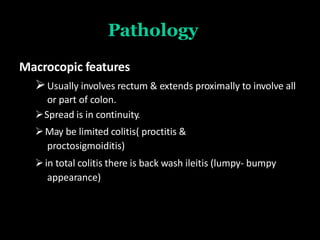
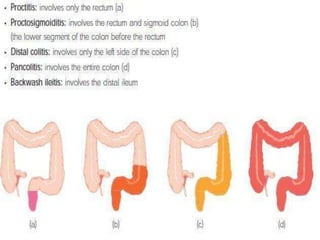
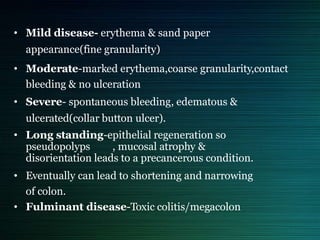
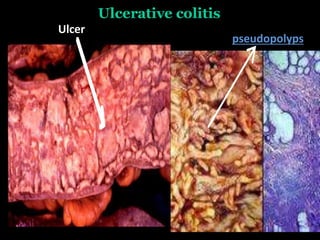
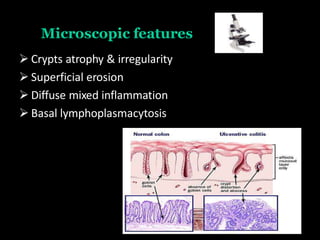
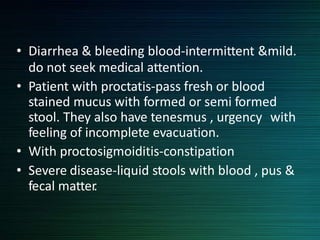
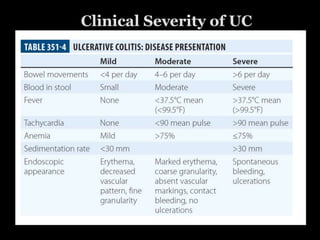
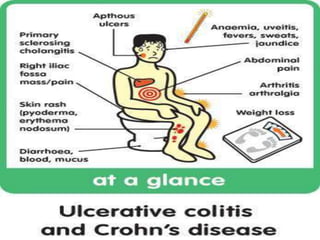
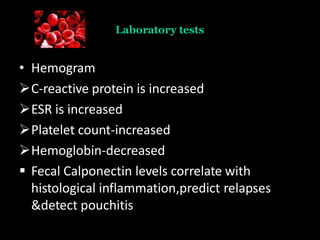
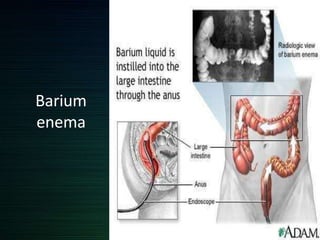
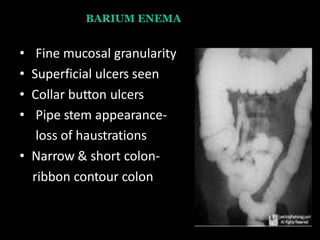
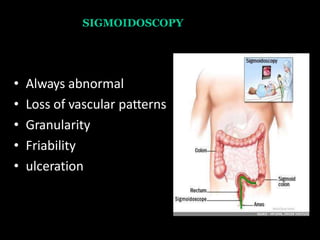
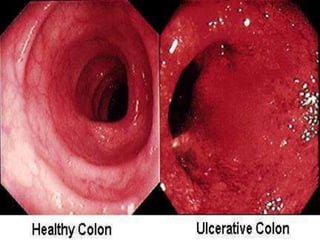
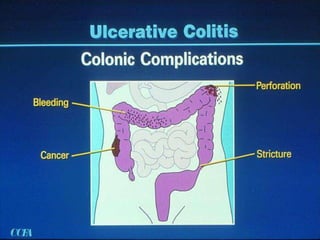
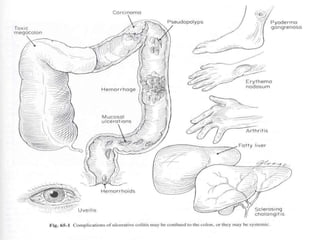
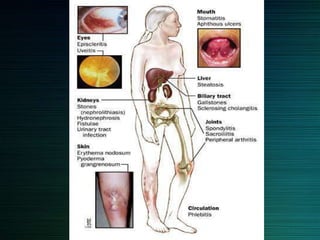
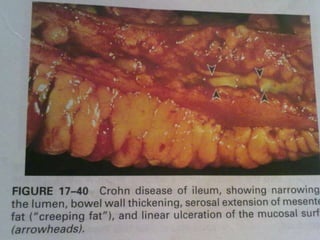
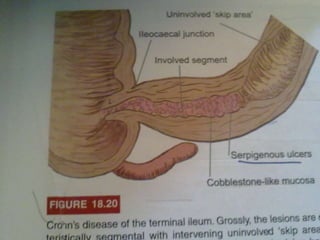
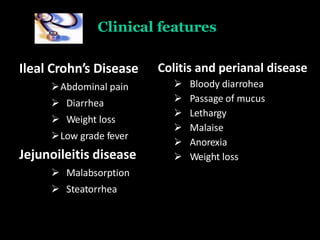
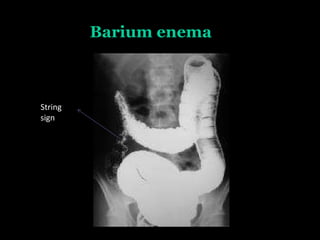
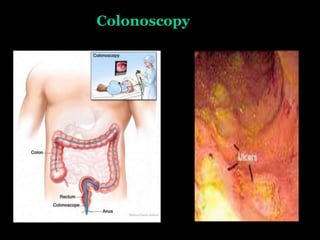
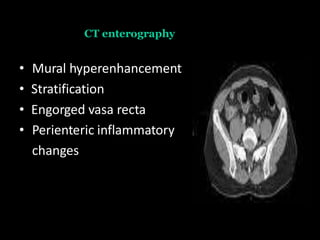
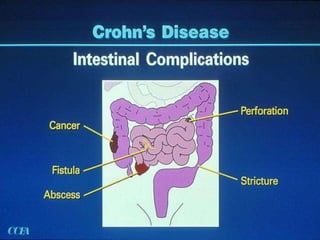
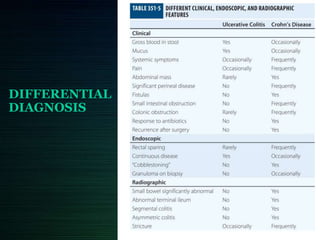
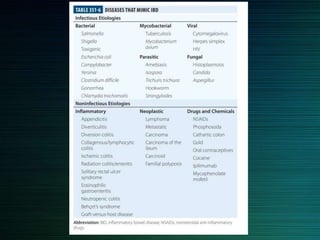
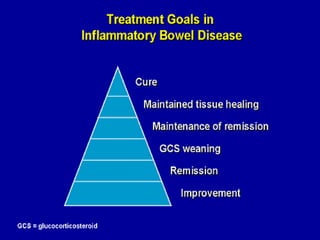
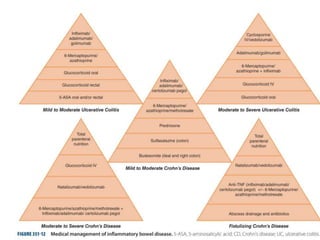
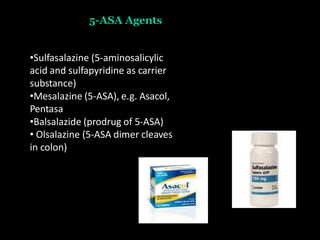
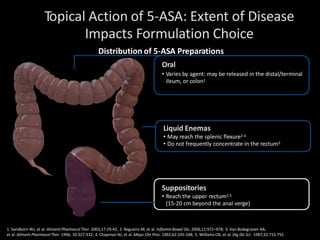
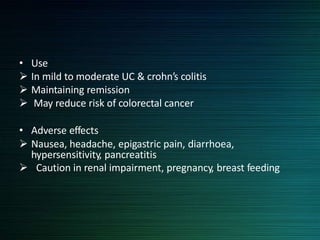
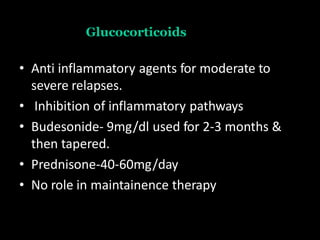
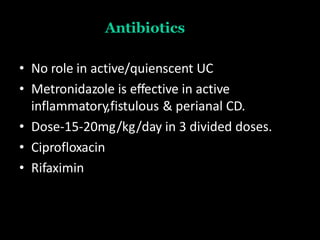
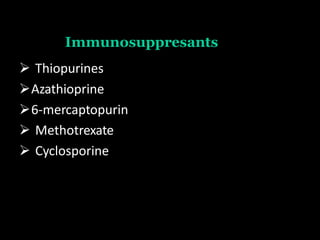
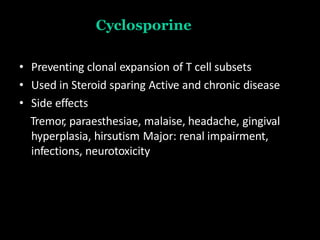
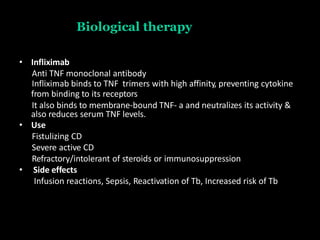
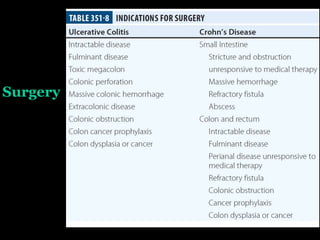
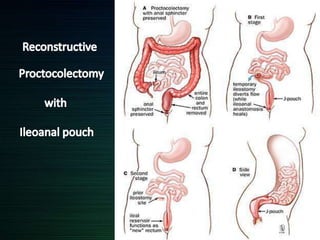
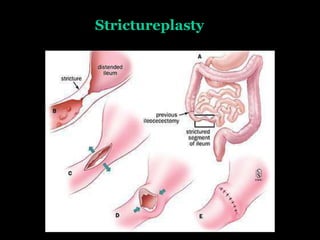
Inflammatory bowel diseases (IBD) include ulcerative colitis and Crohn's disease, which cause chronic inflammation in the intestines. Ulcerative colitis affects only the colon, causing ulcers, while Crohn's disease can impact any part of the digestive tract and deeper layers. Both have no known cause but involve genetic, immune, microbial, and psychosocial factors. Common symptoms are diarrhea, abdominal pain, and rectal bleeding. Diagnosis involves blood tests, endoscopy, imaging, and biopsy. Treatment focuses on medications to reduce inflammation like 5-aminosalicylates, corticosteroids, antibiotics, immunosuppressants, and biological therapies. Surgery may be needed for complications or drug