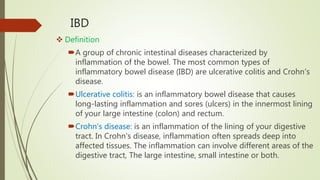
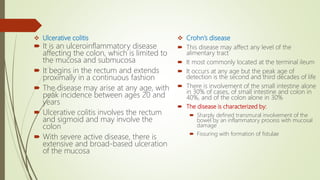
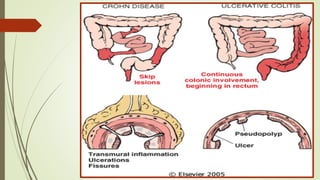
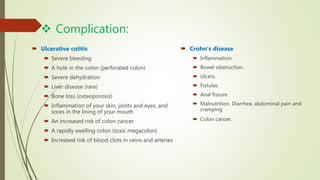
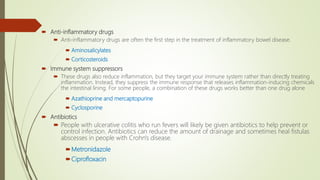
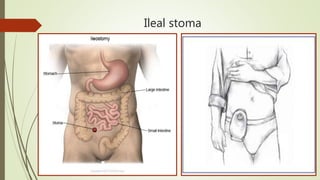
The document discusses inflammatory bowel disease (IBD), which includes ulcerative colitis and Crohn's disease. IBD is characterized by chronic inflammation of the bowel that can affect any part of the gastrointestinal tract from mouth to anus. Common symptoms include abdominal pain, diarrhea, and weight loss. Treatment involves medications to reduce inflammation as well as surgery in severe cases to remove inflamed sections of bowel. Complications can include malnutrition, infection, bowel obstruction, and in rare cases colon cancer. The causes of IBD are not fully understood but involve an abnormal immune response in the gastrointestinal tract.