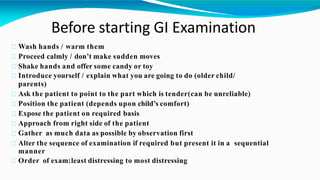
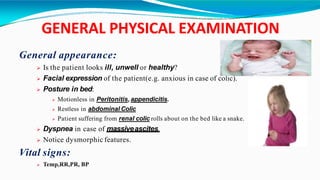
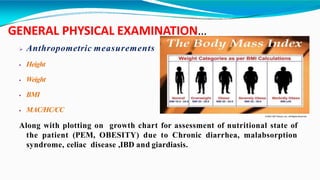
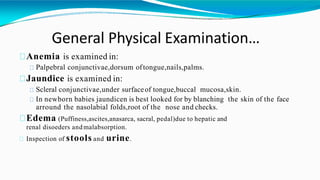
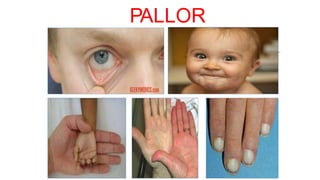
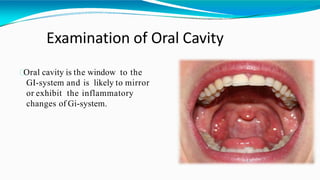
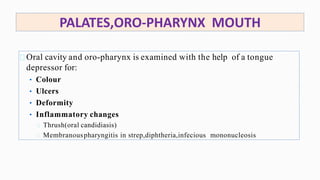
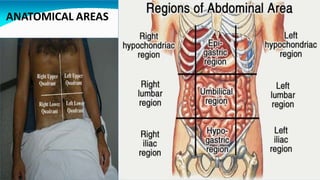
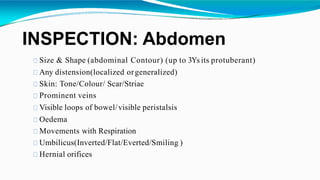
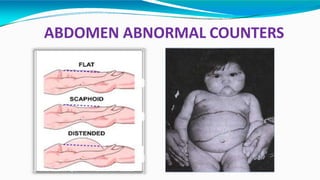
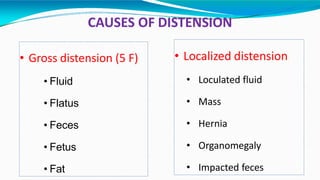
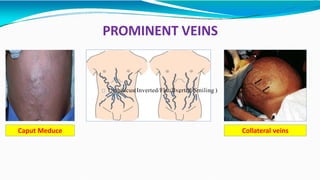
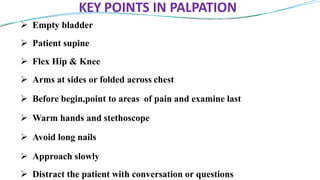
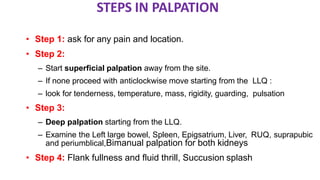
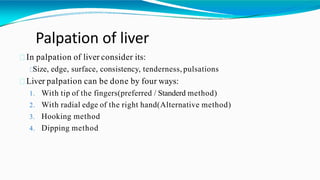
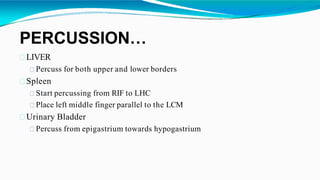
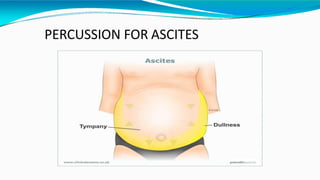
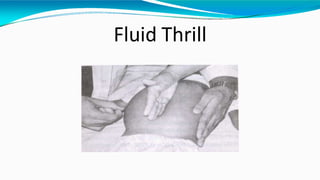
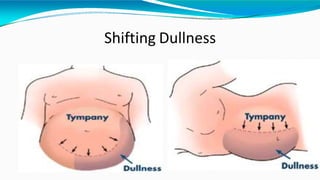
This document provides an overview of pediatric gastrointestinal disorders and examinations. It discusses the anatomy of the GI tract, common signs and symptoms of digestive disorders in children, and specific pediatric GI conditions. It also provides detailed guidance on performing a complete GI examination, including inspection, auscultation, palpation, percussion, and examination of the oral cavity, abdomen, genitalia, and rectum. The goal is to gather all relevant clinical findings through the organized examination of the GI system.











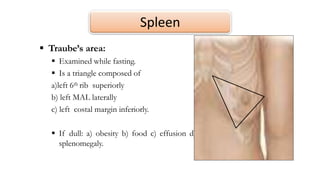
![Spleen
Nixon technique: patient in the right lateral position. Percuss the
upper border in post axillary line. And the lower border obliquely from
below costal margin. [ sensitivity specificity]
Castell technique: patient in the supine position. Percuss the lowest
intercostal space [8th or 9th] in the anterior axillary line. Ask patient to
take strong inspiration during percussion, if dull =splenomegaly. [
sensitivity specificity]
4](https://image.slidesharecdn.com/pediatricgitexamination-200506172605/85/Pediatric-git-examination-72-320.jpg)
![Rectal examination
Normally done in
Acute abdomen
Chronic constipation
Rectal bleeding
Look for
Tone of anal sphincter and tenderness (anal stenosis loose patulous anus
[myelomeningocele], imperforate anus)
Masses ( feces, polyps, teratomas, foreign bodies)
Local abdominal tenderness
Blood or other staining
Rectal prolapse
Perianal area (thread worms, skin tags, protruding polyps, anal fissures, fecal
soiling)](https://image.slidesharecdn.com/pediatricgitexamination-200506172605/85/Pediatric-git-examination-77-320.jpg)
