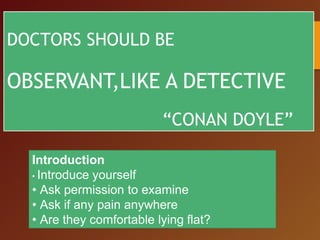
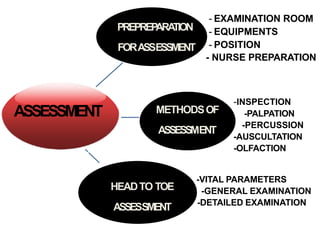
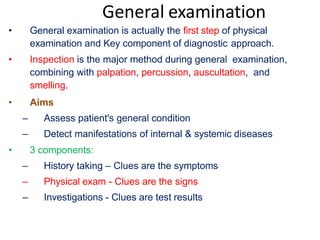
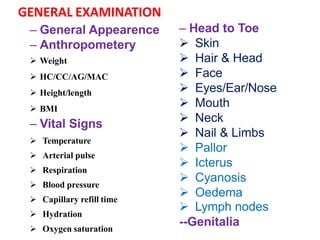
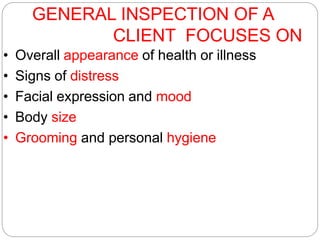
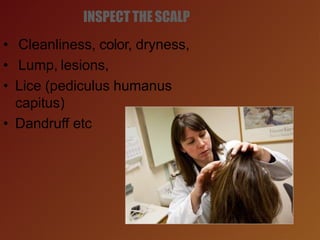
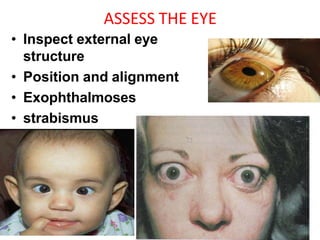
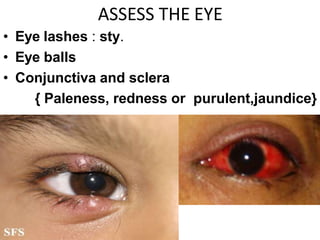
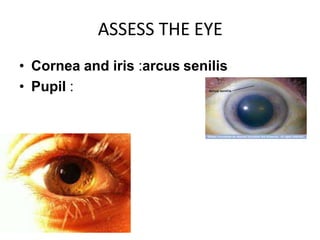
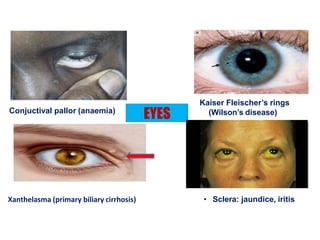
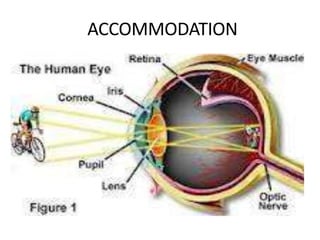
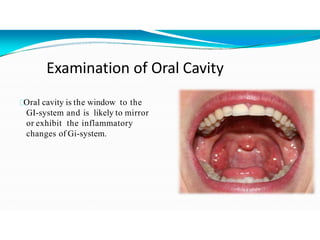
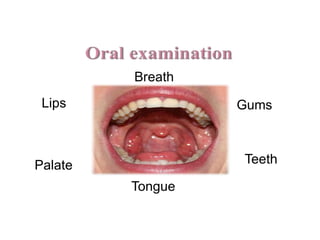
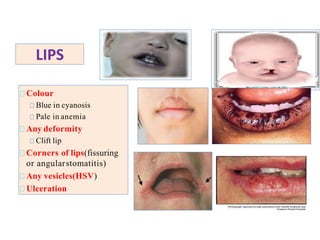
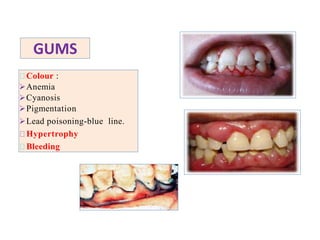
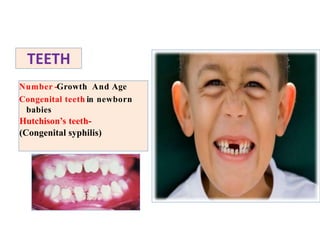
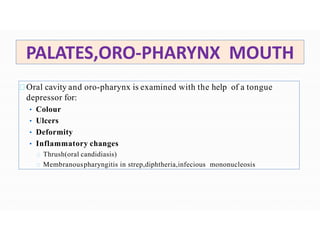
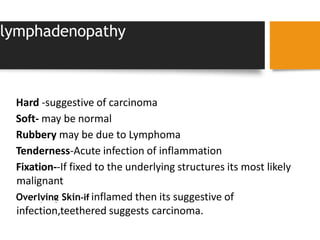
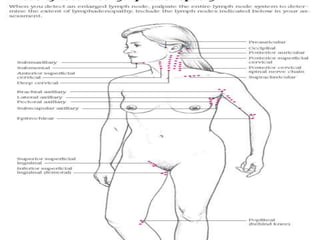
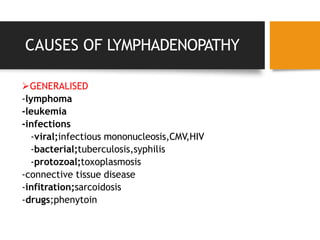
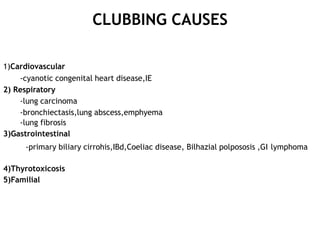
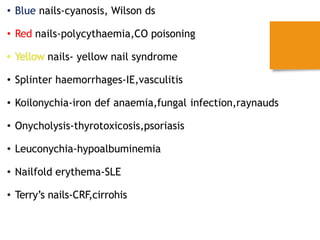
Doctors should carefully observe patients like detectives during physical examinations. The document outlines the process of a physical assessment including preparation, examination methods, and conducting assessments from head to toe. Key steps involve introducing oneself, obtaining permission before examining, asking about pain or discomfort, inspecting various body systems, and documenting findings and vital signs. Physical assessments provide objective health information through direct observation and examination techniques.