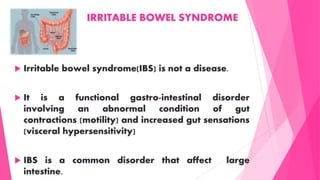
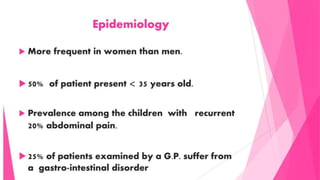
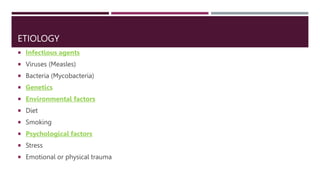
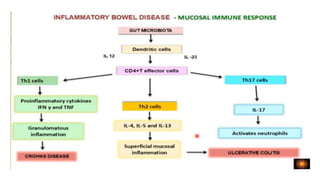
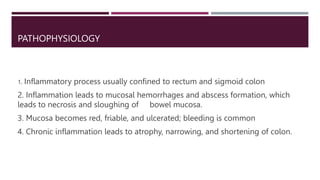
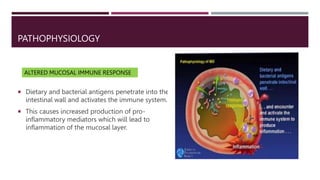
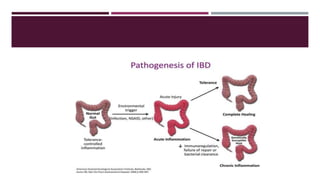
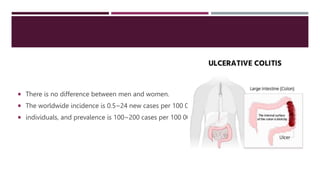
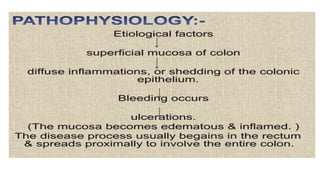
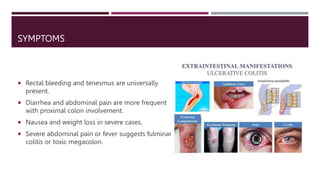
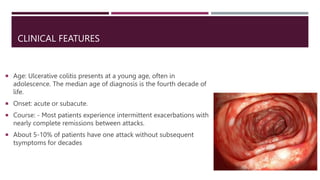
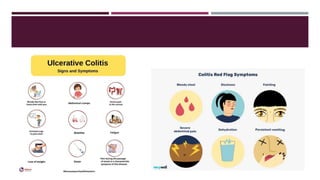
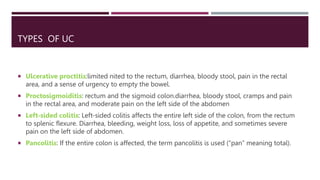
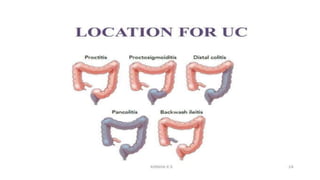
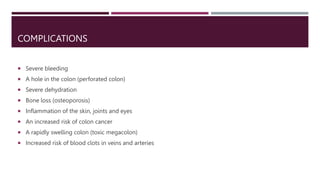
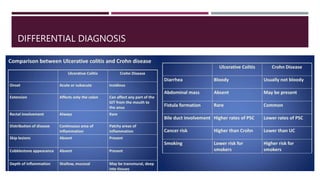
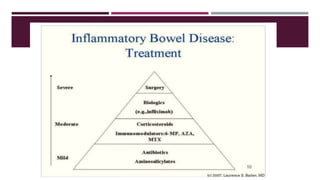
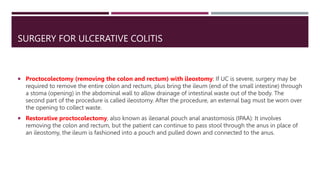
The document discusses inflammatory bowel disease (IBD), specifically ulcerative colitis, detailing its definition, classification, etiology, pathophysiology, symptoms, diagnosis, treatment options including pharmacological and surgical interventions, as well as Ayurvedic management. It emphasizes the chronic nature of the disease, the importance of differentiating it from other conditions, and the need for long-term management to induce and maintain remission. Complications of ulcerative colitis and various types and symptoms associated with it are also outlined.