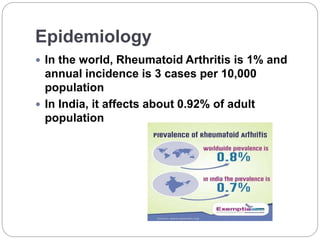
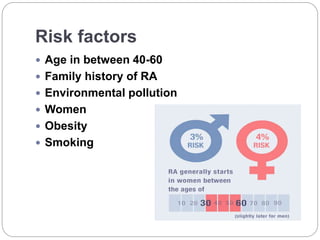
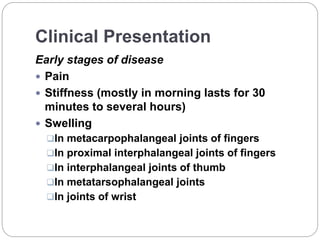
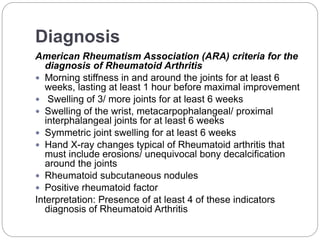
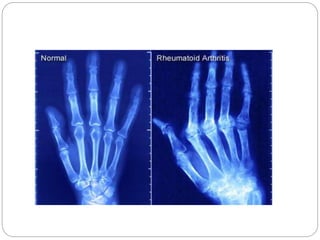
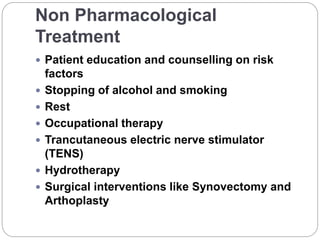
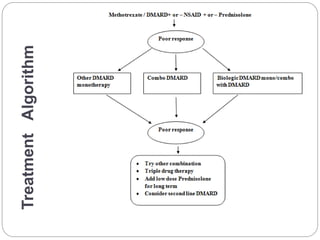
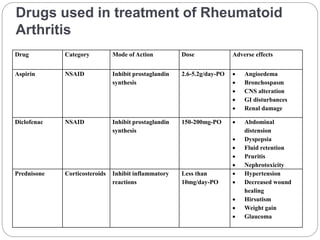
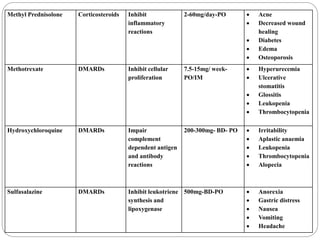
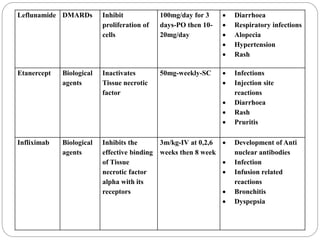
Rheumatoid arthritis is an autoimmune disease that causes inflammation, swelling, and pain in the joints. It affects approximately 1% of the world's population and 0.92% of the adult population in India. There are two main types - seropositive RA, where the body produces immune reactions to normal tissue, and seronegative RA, where tests for rheumatoid factor and anti-CCP antibodies are negative. Risk factors include age 40-60, family history, smoking, obesity, and female sex. Diagnosis involves evaluating symptoms, x-rays of affected joints, and blood tests for rheumatoid factor and anti-CCP antibodies. Treatment includes non-pharmacological therapies as well as drugs like