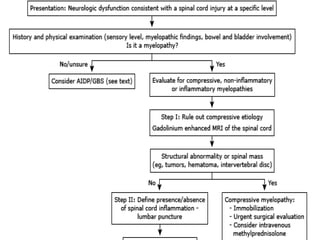
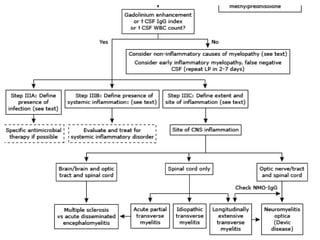
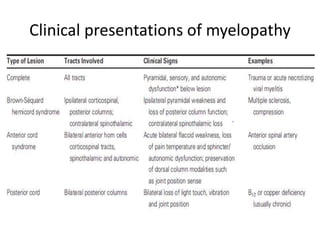
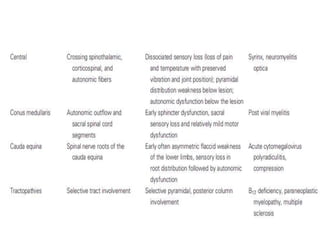
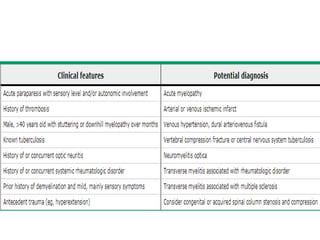
This document discusses the approach to transverse myelitis (TM). Some key points:
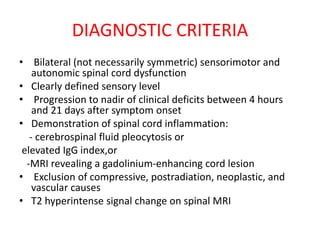
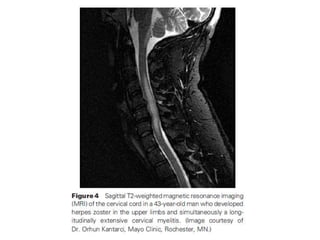
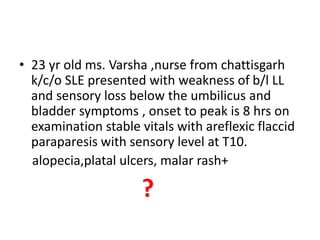
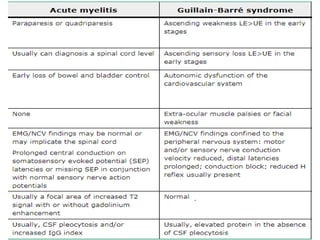
1. TM is an acute inflammatory disorder of the spinal cord that presents with weakness, sensory alterations, and bowel/bladder dysfunction. Symptoms progress to maximum deficit within 4 hours to 21 days.
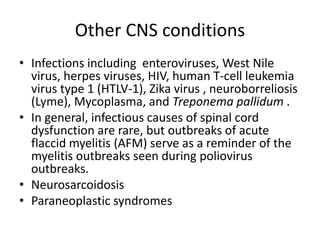
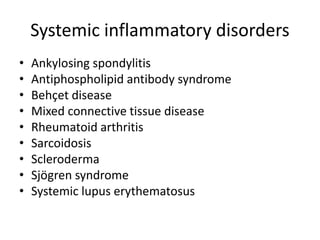
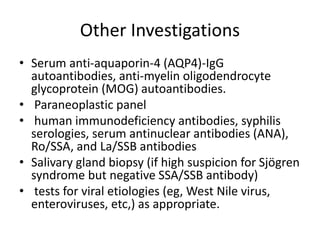
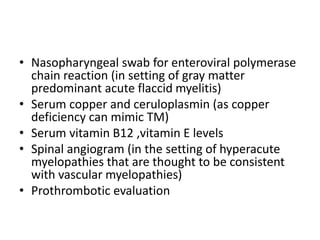
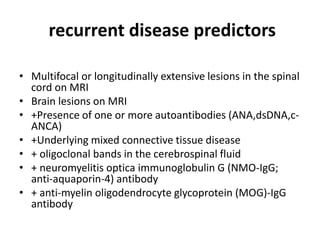
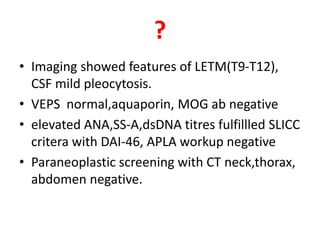
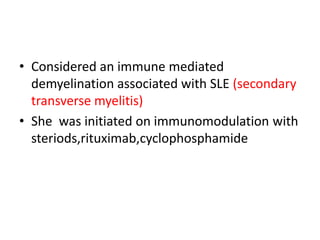
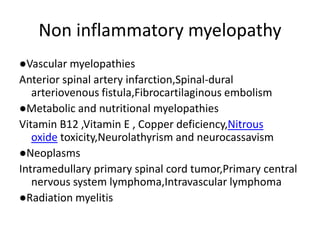
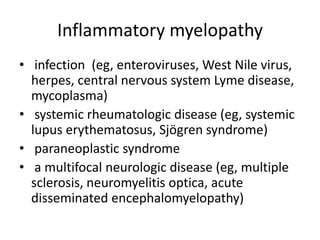
2. It can be idiopathic or secondary to conditions like multiple sclerosis or systemic lupus erythematosus (SLE). Diagnosis involves ruling out other causes and detecting spinal cord inflammation.
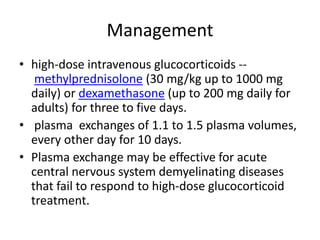
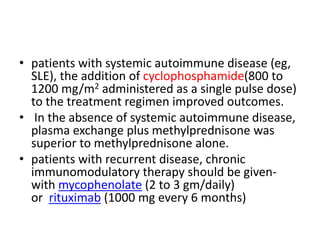
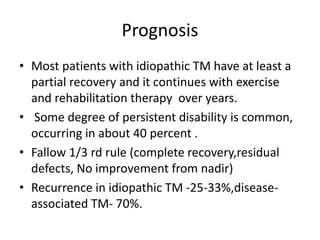
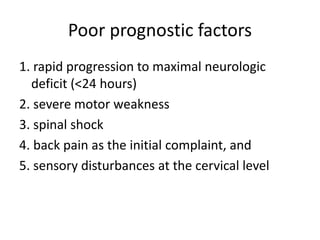
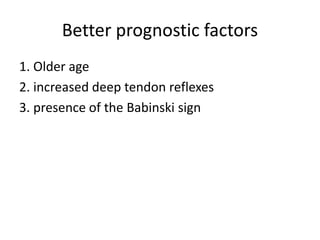
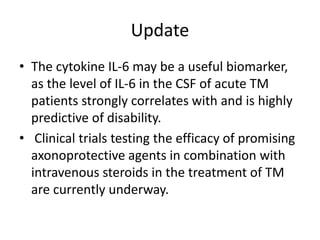
3. Initial treatment involves high-dose steroids and possibly plasma exchange. Patients with underlying autoimmune diseases may require additional immunotherapy. Prognosis depends on factors like severity and speed of progression, with most recovery
![• Idiopathic TM usually occurs as a postinfectious complication and
appears to result from an autoimmune process.
• Secondary TM
• Acquired central nervous system autoimmune disorders that can
cause TM include :
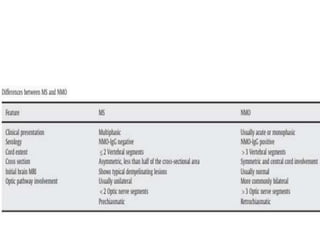
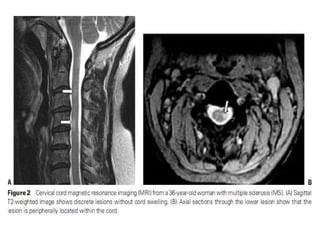
• TM as a part of the spectrum of multiple sclerosis. In some cases,
TM is the initial demyelinating event (a clinically isolated syndrome
[CIS]) that precedes clinically definite multiple sclerosis.
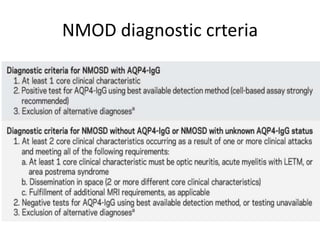
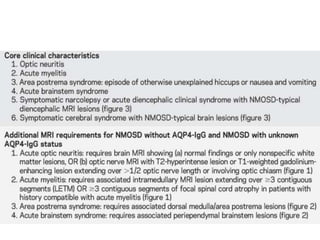
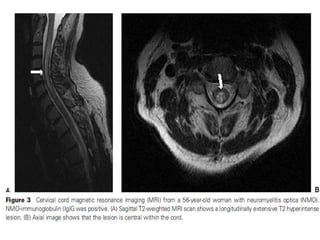
• TM manifesting as a neuromyelitis optica spectrum disorder.
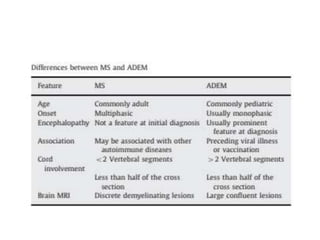
• TM may be seen in patients with acute disseminated
encephalomyelitis, a monophasic demyelinating disease with
multifocal neurologic symptoms and encephalopathy.](https://image.slidesharecdn.com/transveremyelitis-200512052912/85/Transvere-myelitis-18-320.jpg)