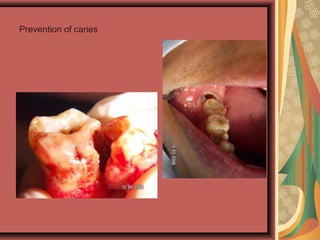
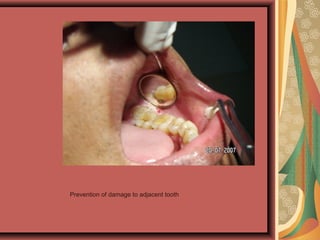
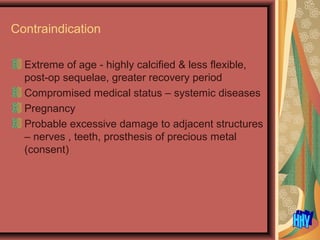
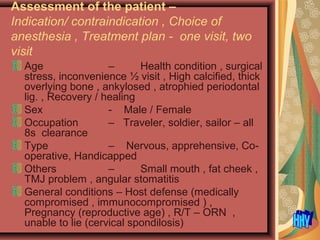
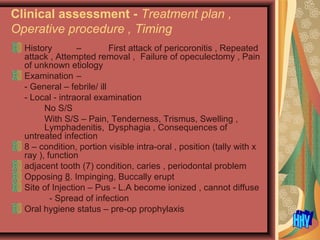
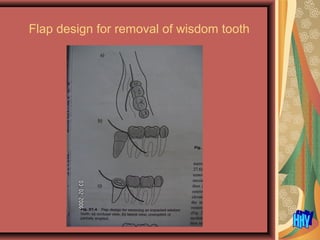
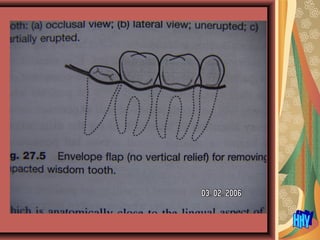
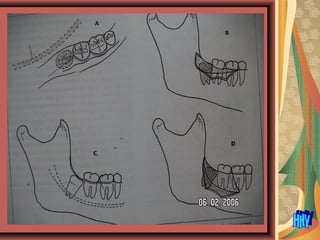
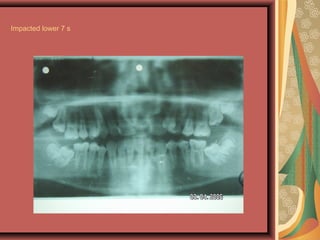
This document discusses impacted teeth, specifically impacted third molars (wisdom teeth). It begins by defining impacted teeth and listing common causes, including local factors like lack of space and systemic factors like rickets.
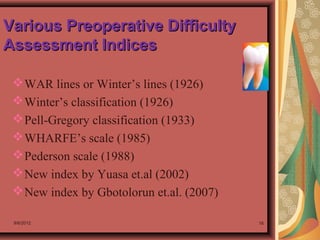
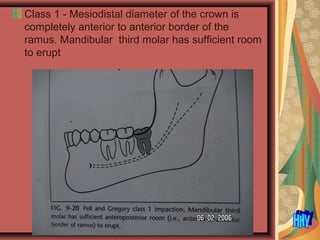
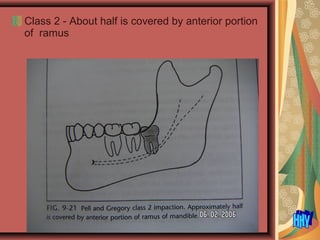
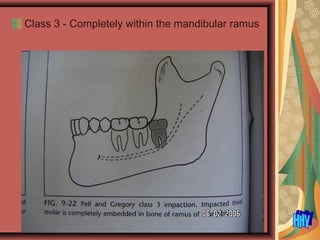
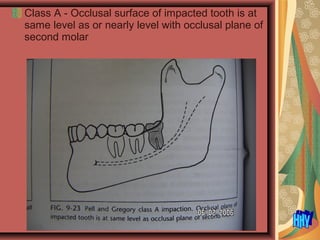
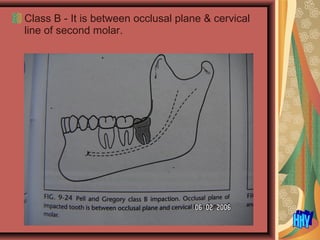
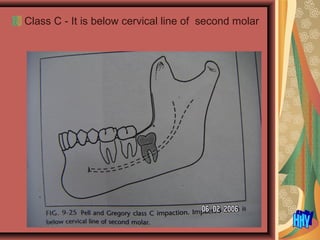
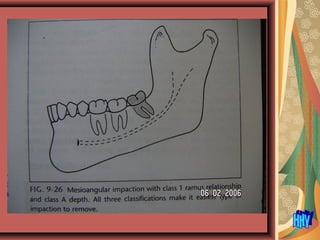
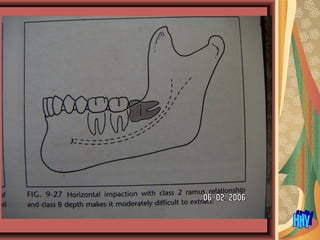
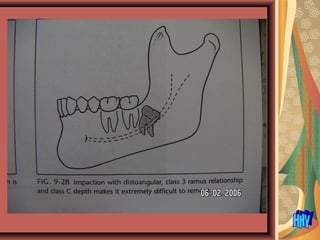
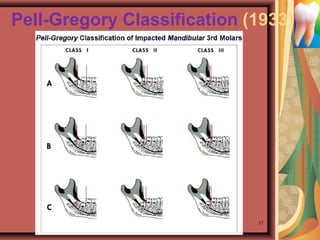
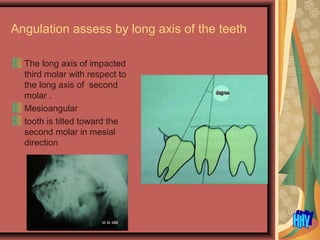
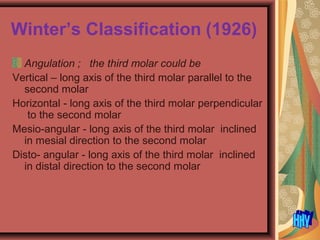
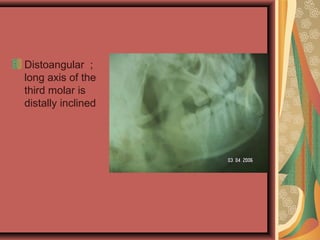
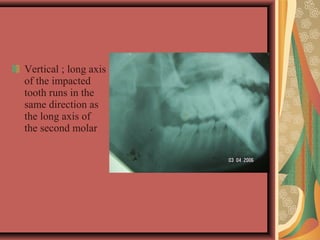
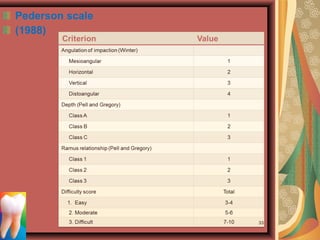
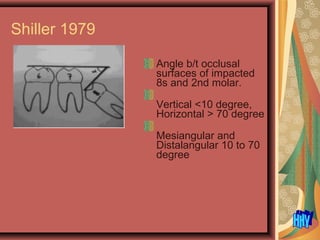
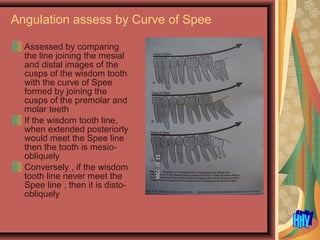
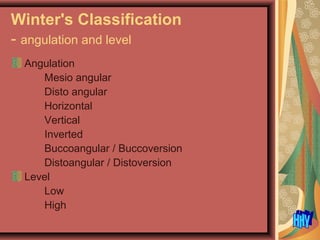
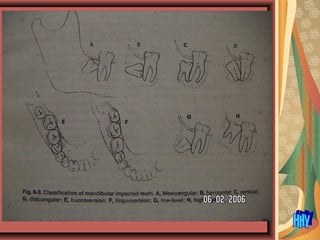
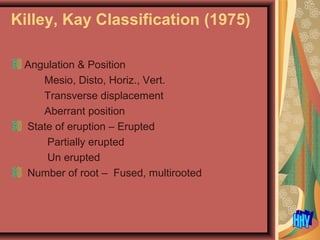
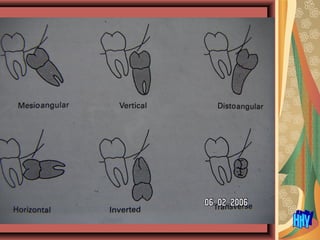
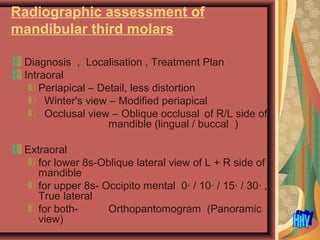
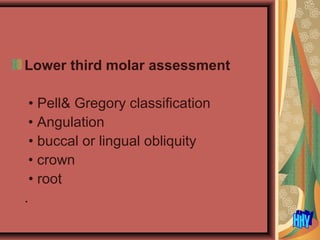
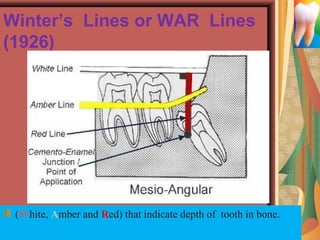
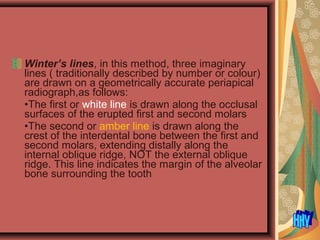
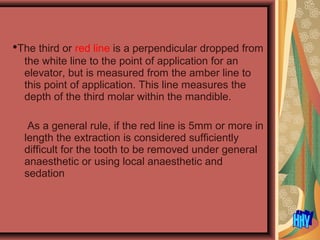
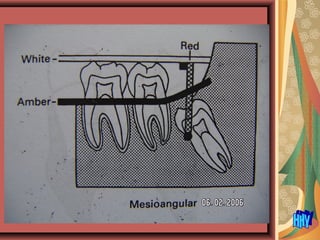
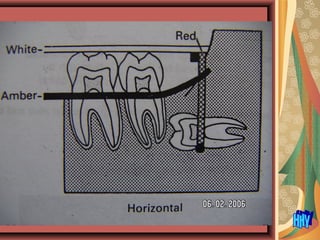
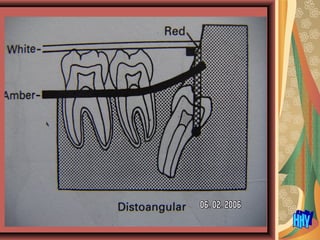
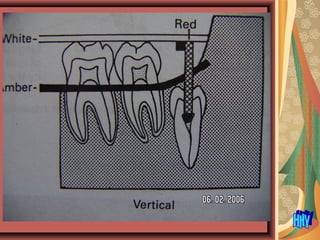
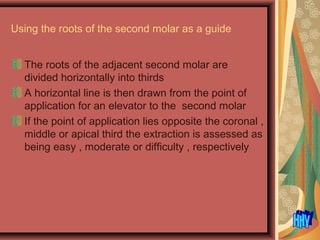
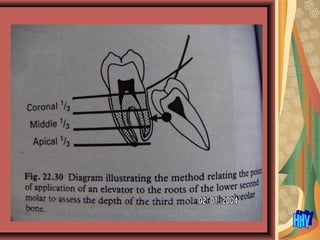
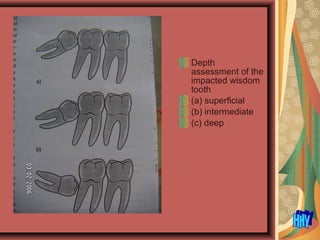
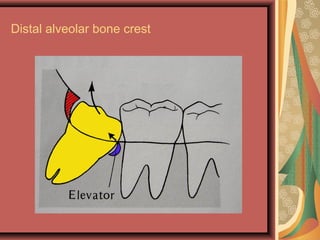
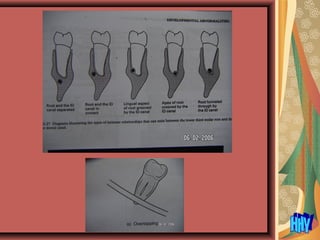
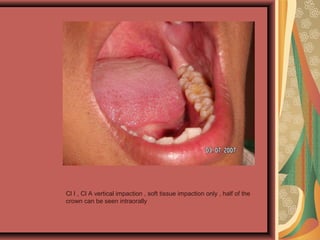
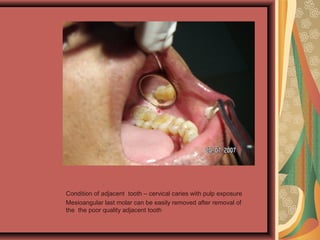
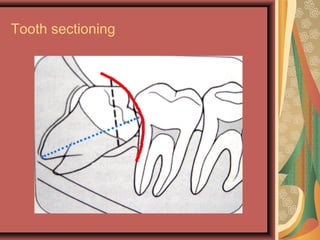
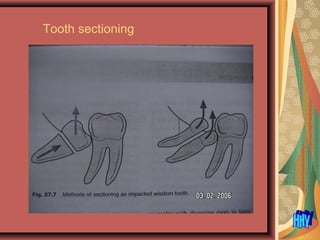
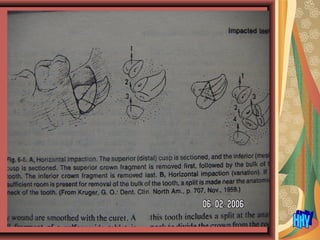
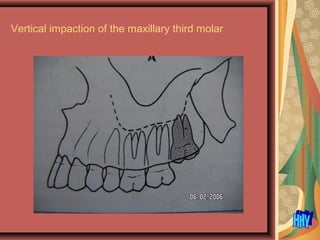
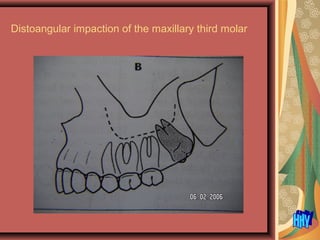
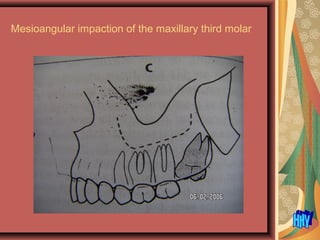
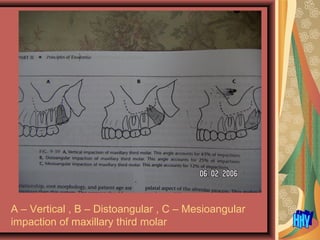
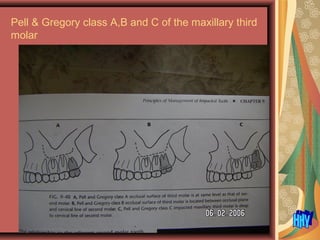
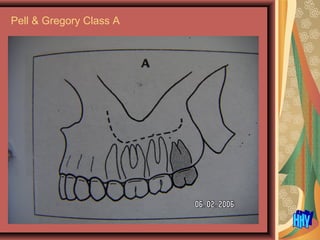
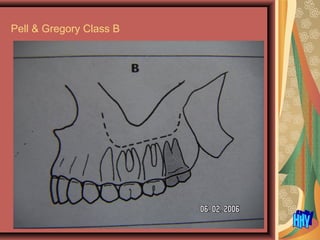
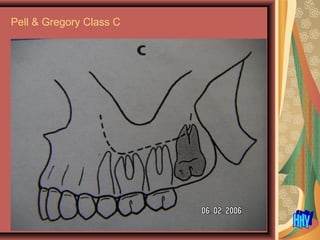
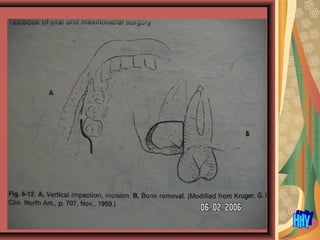
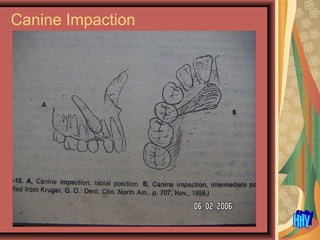
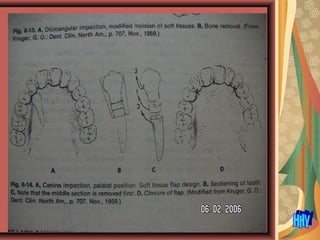
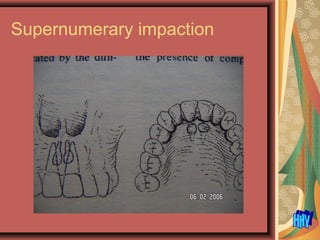
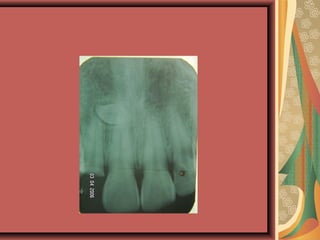
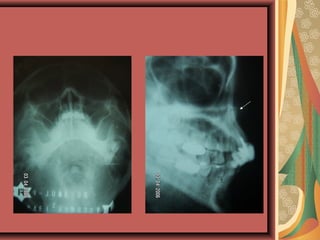
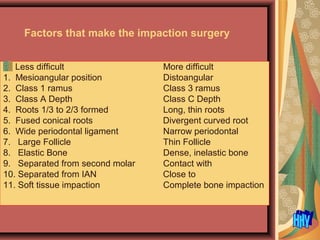
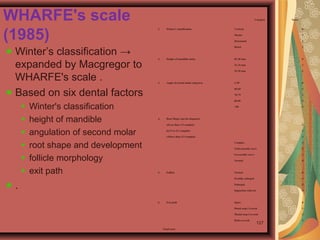
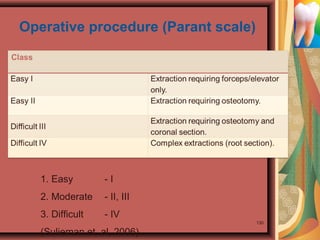
It then discusses methods for assessing impacted teeth, including the Pell-Gregory and Winter's classifications which examine location, angulation, and depth of impaction. Common angulation types like mesioangular, vertical, and horizontal are defined. Diagnostic imaging tools for evaluating impacted teeth are also outlined.
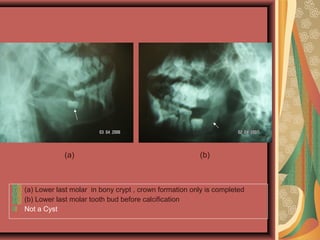
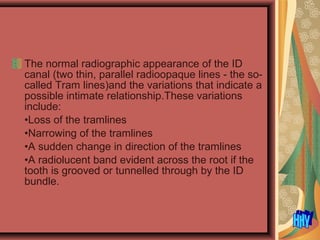
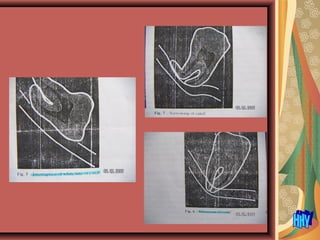
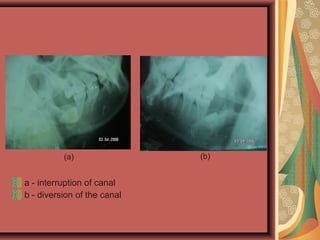
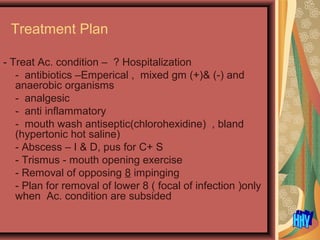
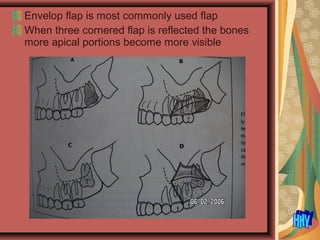
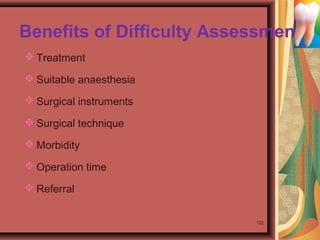
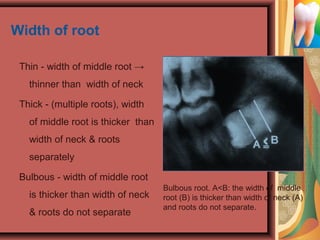
The document concludes by noting that radiographic assessment of impacted third molars is important for diagnosis, treatment planning, and identifying any relationship between the tooth roots and the inferior dental canal. Depth of impaction