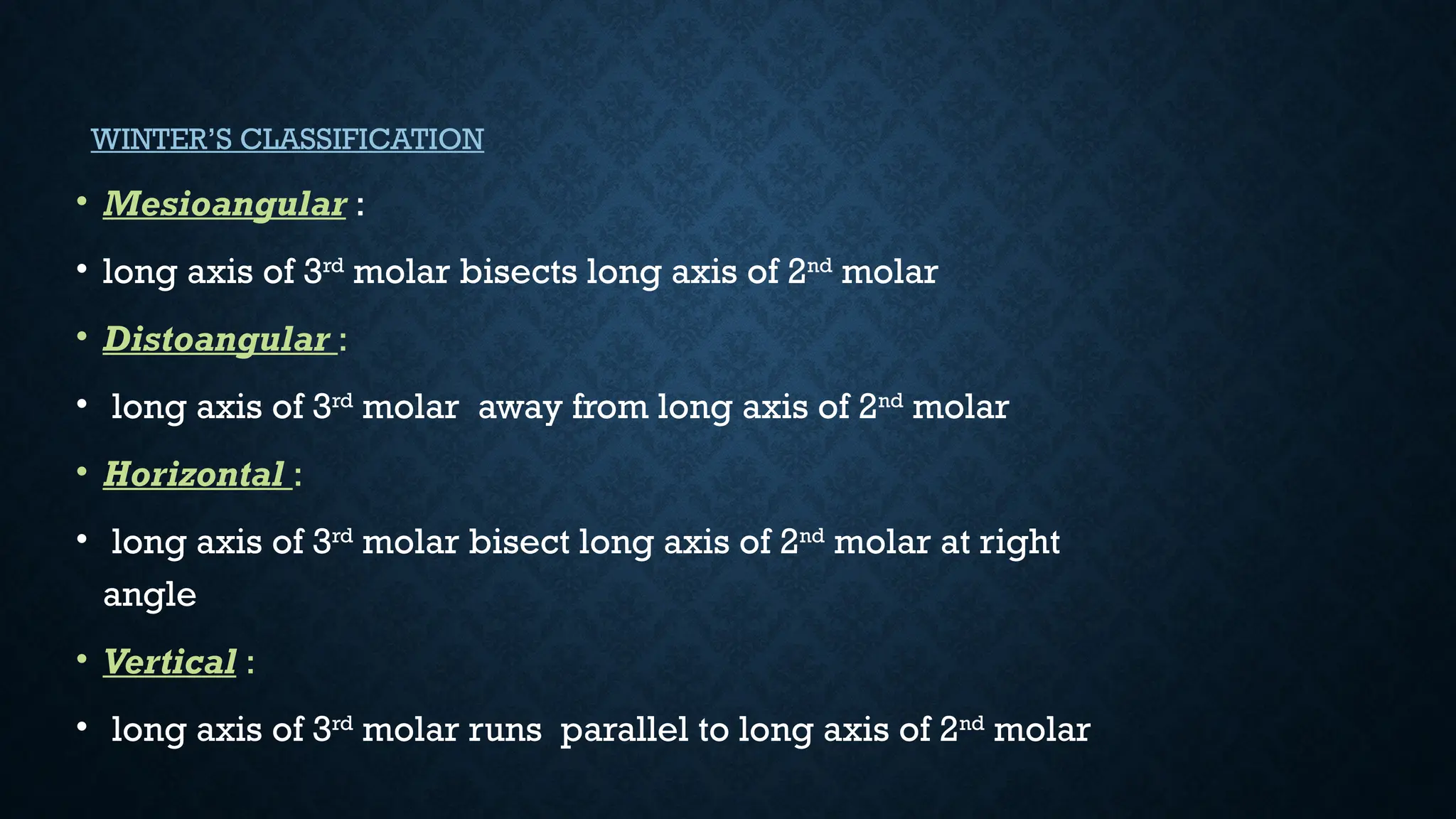
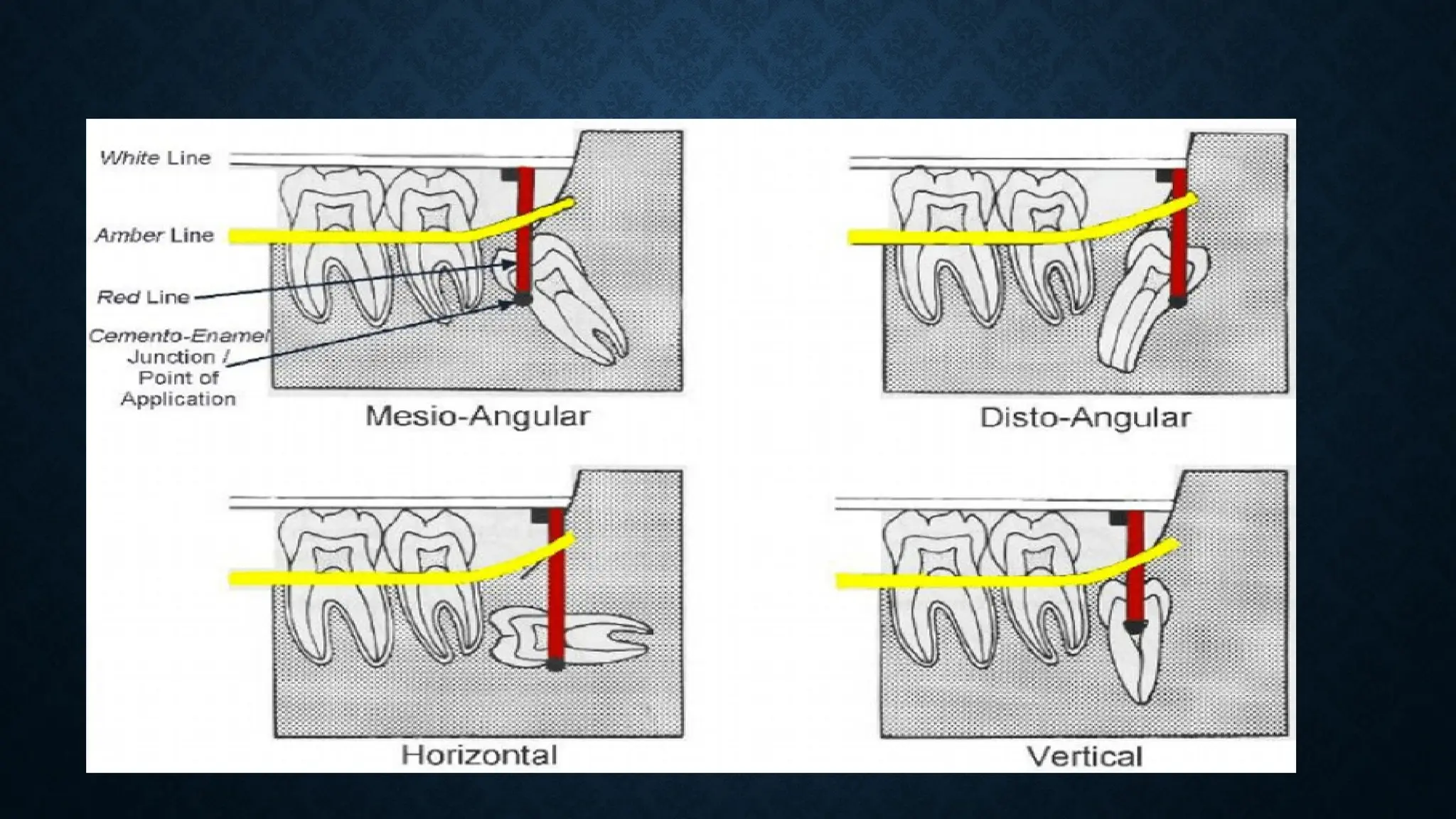
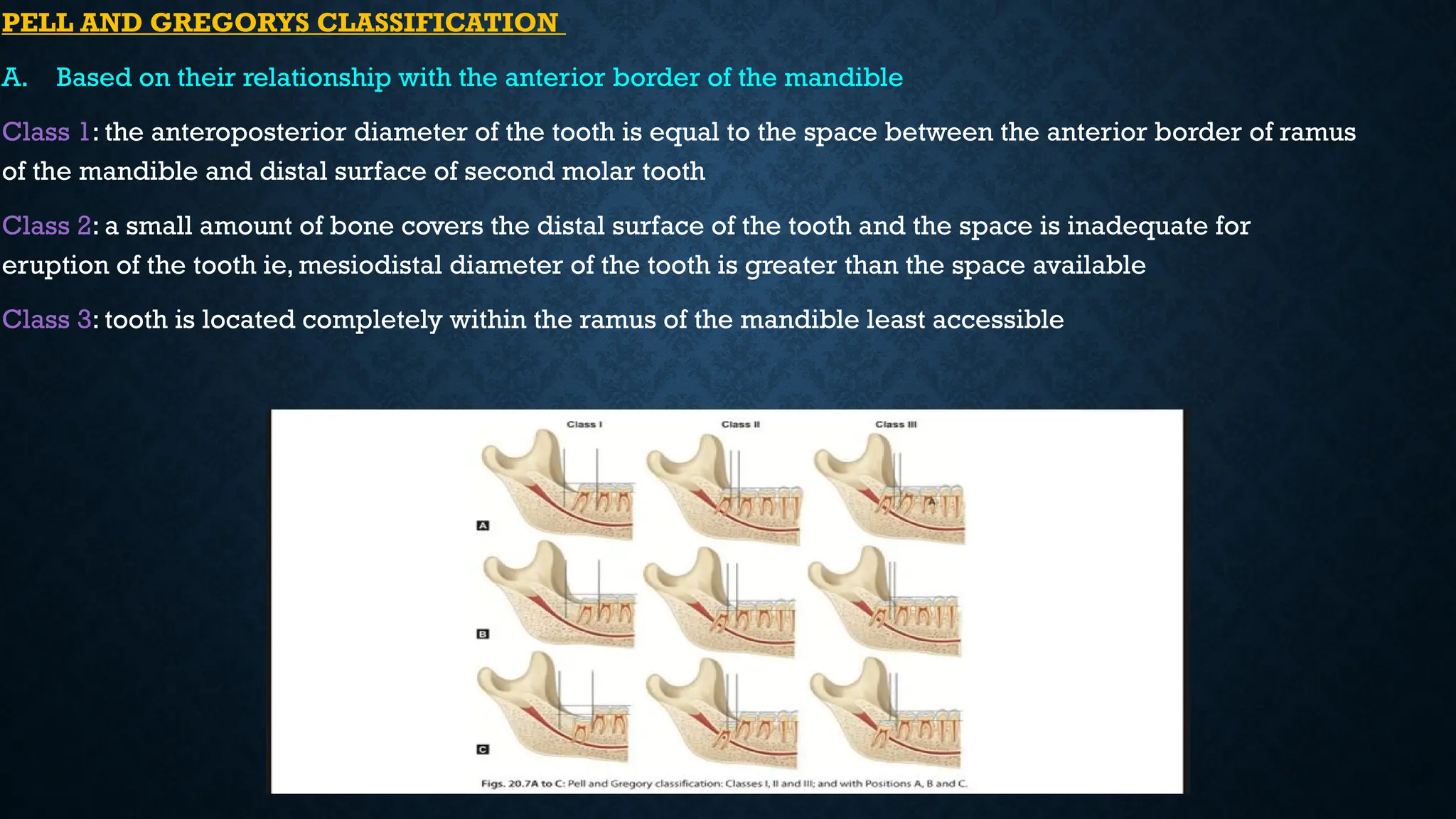
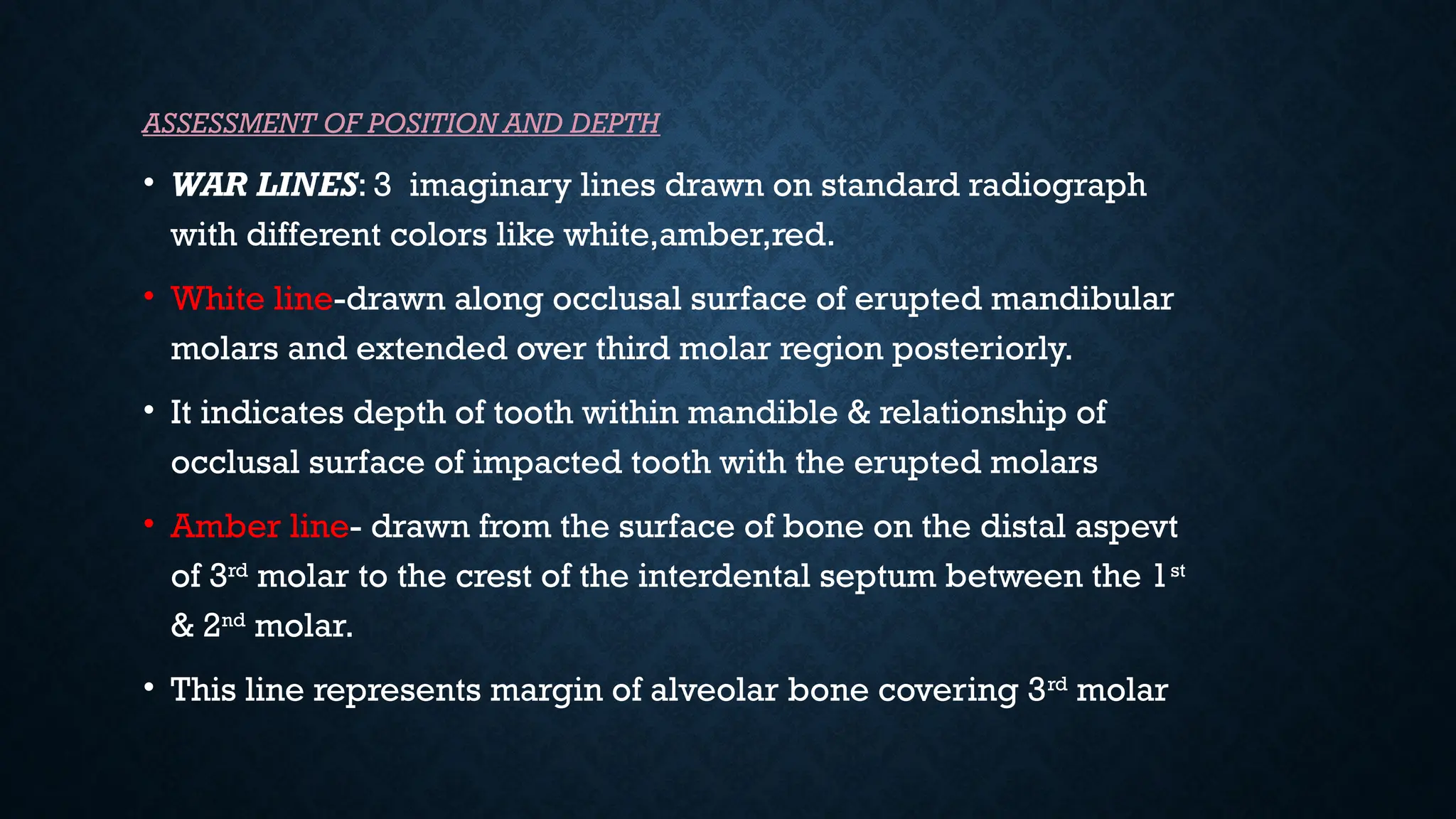
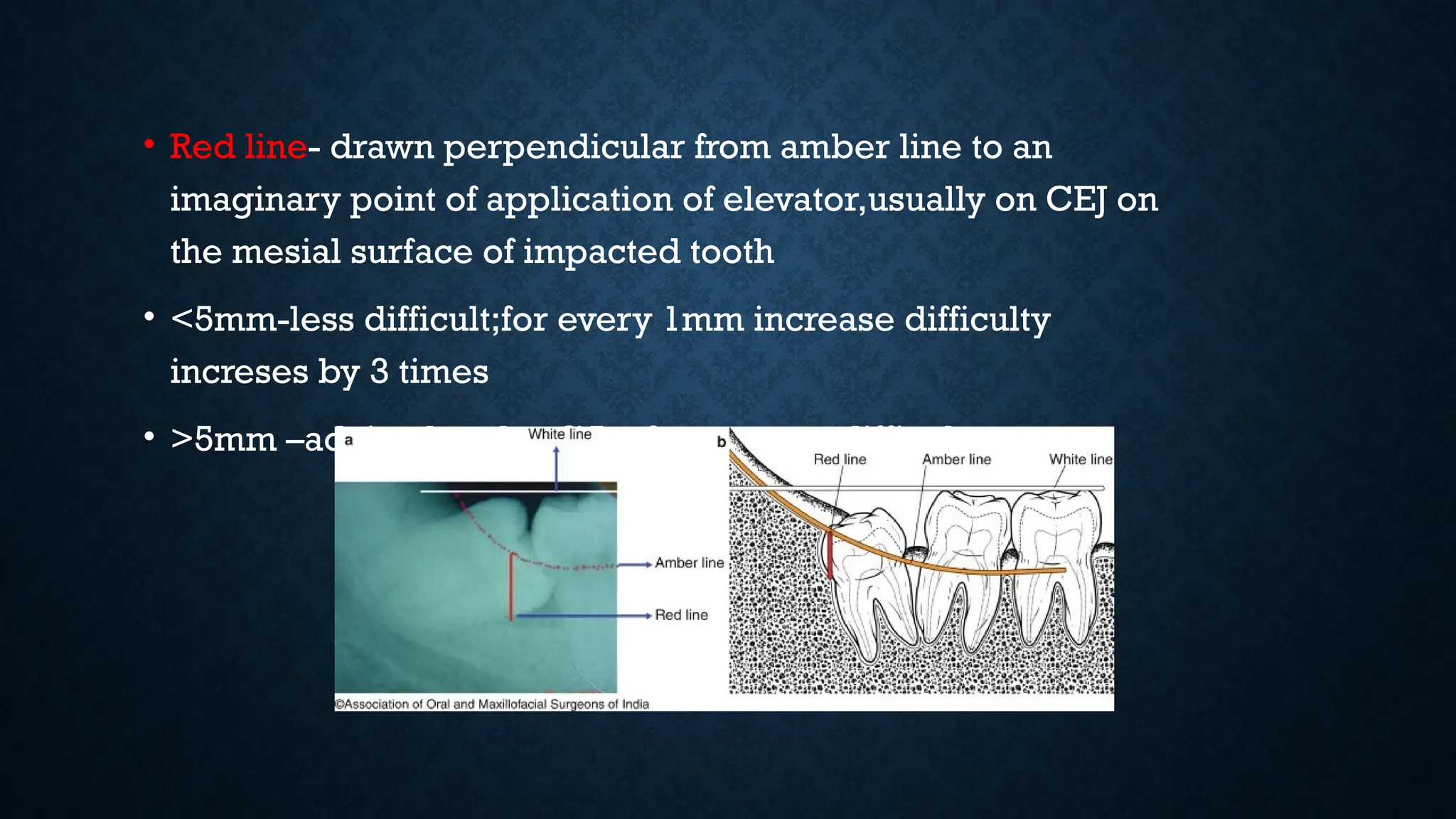
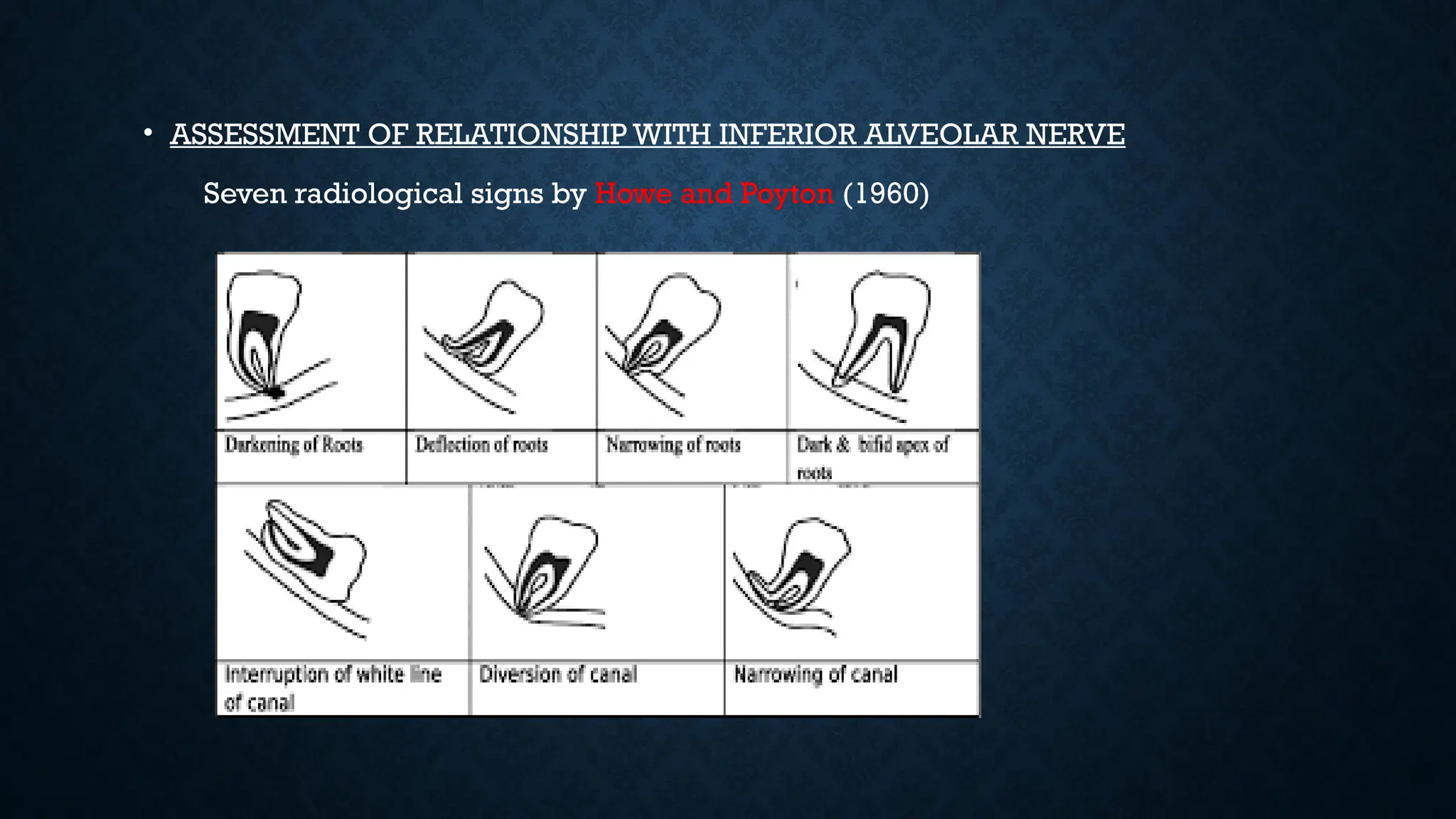
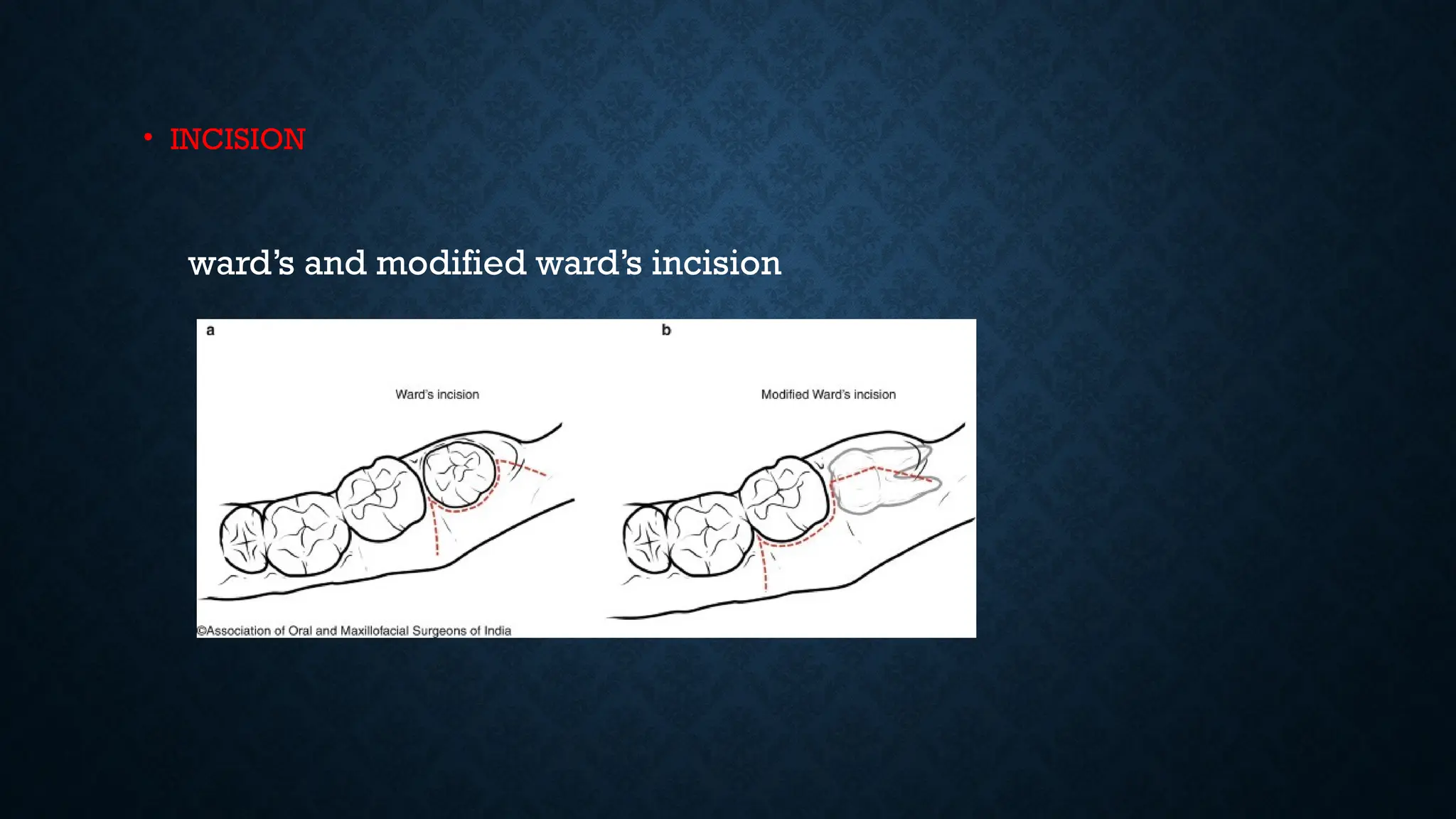
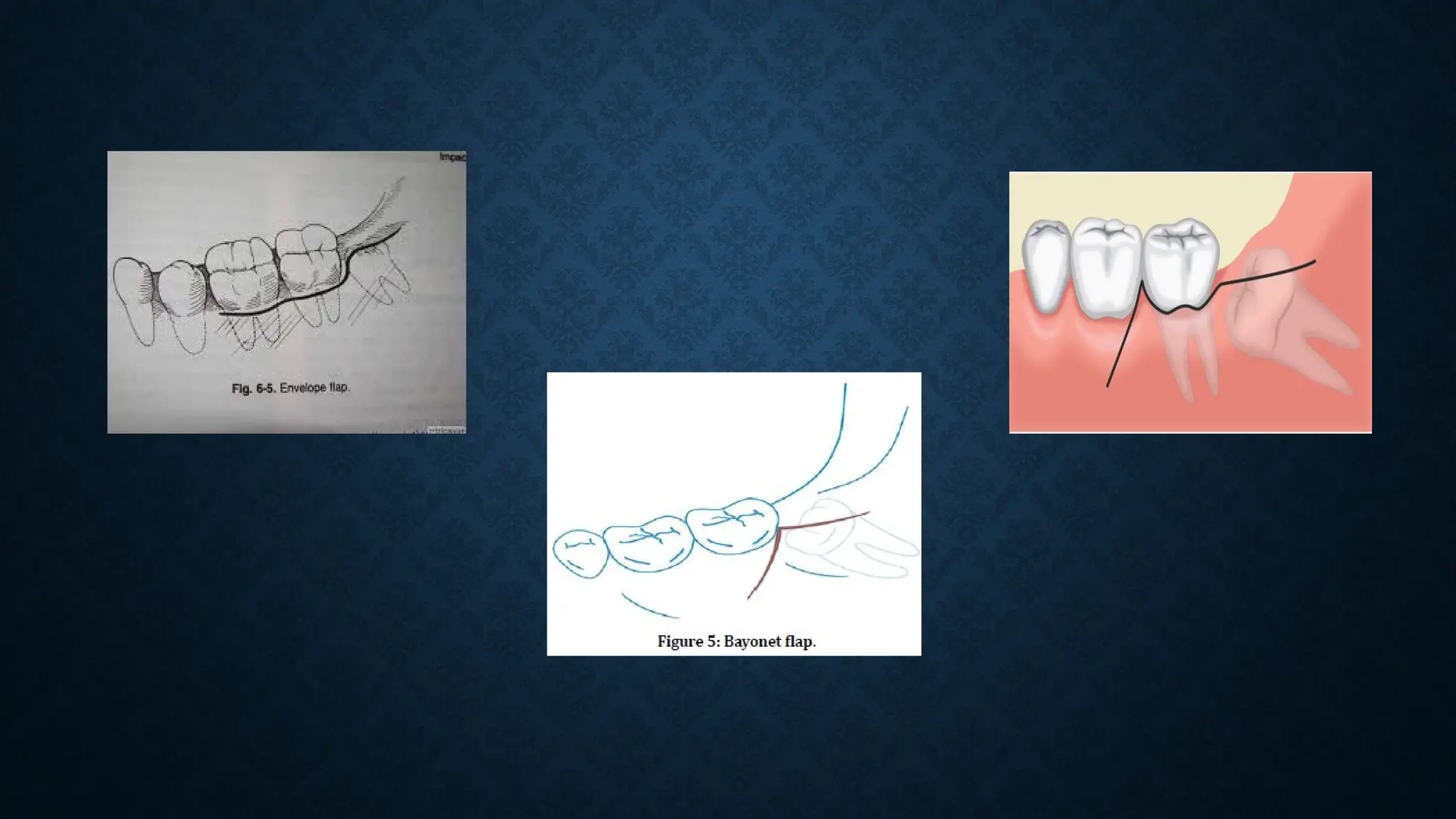
The document discusses the impaction of mandibular third molars, including its definition, causes, indications and contraindications for removal, as well as surgical techniques for extraction. Various theories of impaction are presented, along with classifications based on anatomical relationships and clinical evaluations necessary for management. It emphasizes the importance of timely intervention in cases of impaction to avoid complications associated with delayed removal.