The document discusses impacted third molars, including their classification, surgical removal procedure, and potential complications. It begins with definitions of tooth impaction and discusses causes such as insufficient jaw space. It then covers classification systems involving angulation, depth, and relationship to surrounding structures. Indications for removal include recurrent infections, cysts/tumors, and facilitating other procedures. The surgical procedure is outlined in steps including incisions, bone removal, tooth sectioning and extraction. Risks like nerve injury are also addressed based on radiographic findings. In summary, the document provides an overview of impacted third molar diagnosis, treatment planning, surgical techniques and considerations.





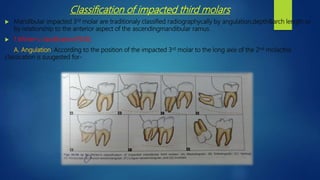
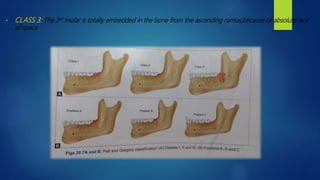
![ B.Depth: As per the relationship to the occlusal surface of the adjoining 2nd molar of the impacted mandibular 3rd molar,the
depth can be judged:
• Position A: The highest position of the tooth is on a level with or above the occlusal line.
• Position B: The highest position of the tooth is below the occlusal plane,but above the cervical level of 2nd molar.
• Position C: The highest position of the tooth is below the cervical level of the 2nd molar.
2.Pell and Gregory classification(1933):
• Relationship of the impacted lower 3rd molar to the ramus of the mandible &the 2nd molar[based on the space available distal
to the second molar]:
• CLASS 1:Sufficient space available between the anterior border of the ascending ramus &the distal side of the 2nd molar for
the eruption of the 3rd molar.
• CLASS 2: The space available between the anterior border of the ramus & the distal side of the second molar is less than
mesiodistal width of the crown of the 3rd molar,It denotes that,distal portion of the 3rd molar crown is covered by the bone
from the ascending ramus.](https://image.slidesharecdn.com/osfinalyear-200405123235/85/Mandibular-3rd-molar-impacion-9-320.jpg)