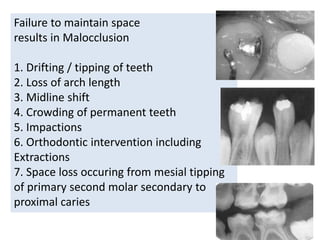
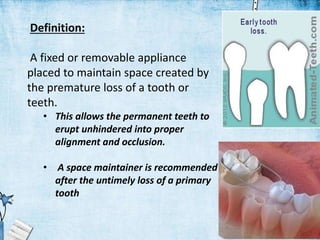
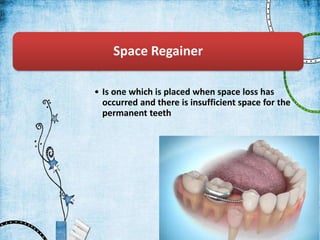
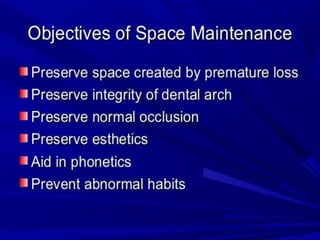
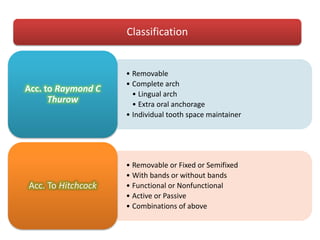
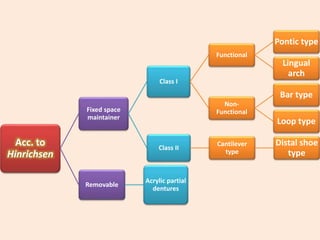
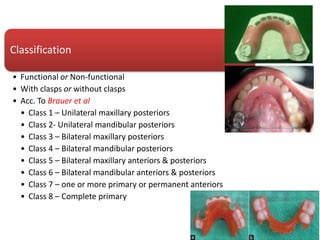
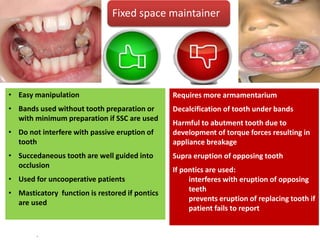
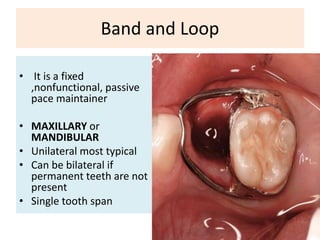
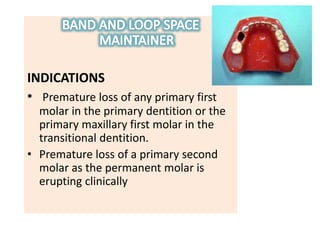
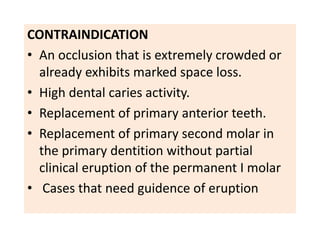
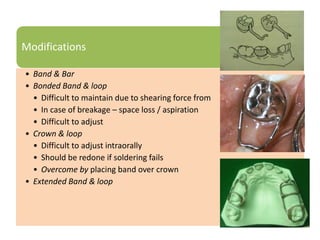
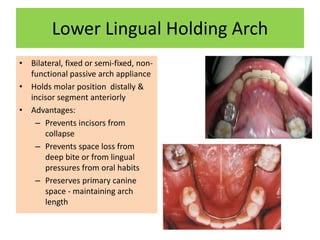
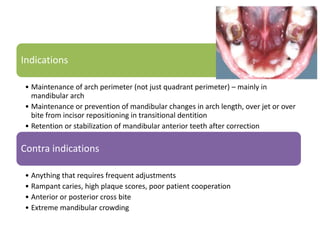
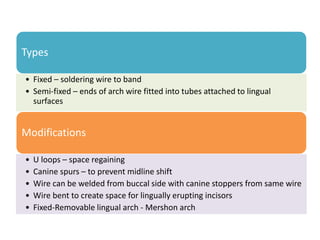
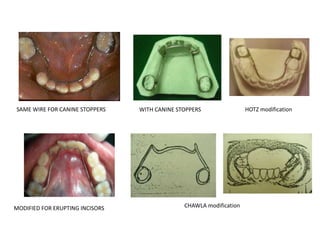
This document discusses space maintainers, which are appliances used to maintain space for permanent teeth after premature loss of primary teeth. It describes different types of space maintainers including removable, fixed, lingual arch, and distal shoe appliances. Key factors in planning space maintenance like dental age and sequence of eruption are outlined. The document summarizes indications, contraindications, advantages and disadvantages of various space maintainer designs. Space maintainers aim to guide proper eruption of permanent teeth into ideal alignment and occlusion.




![• If not removed before
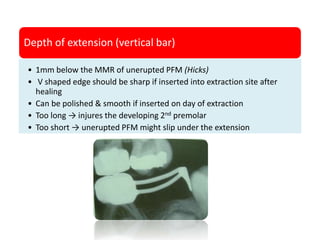
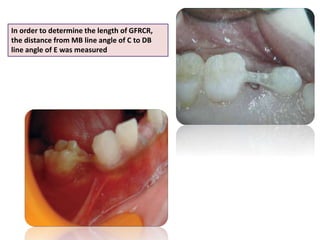
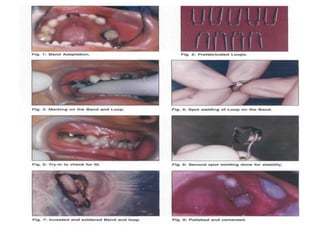
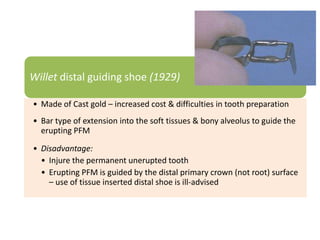
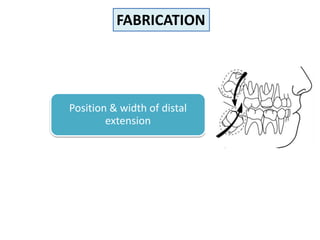
A] Measuring the 2nd primary molar
• distance between distal surface of primary 1st molar & unerupted
PFM (if already missing)
• May force the tooth to erupt too far distally (if fabricated at 3 to 4
years of age) → disto-occlusion of molars
B] Measured from the radiograph
Length of distal extension (horizontal bar)](https://image.slidesharecdn.com/spacemaintainerashli-160612104001/85/Space-maintainers-34-320.jpg)