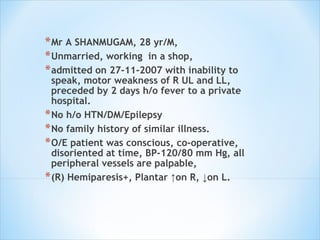
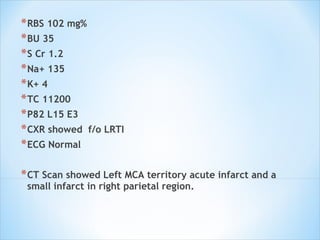
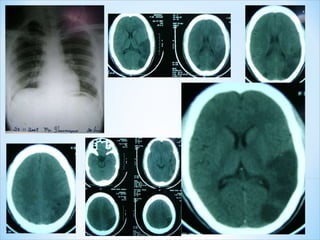
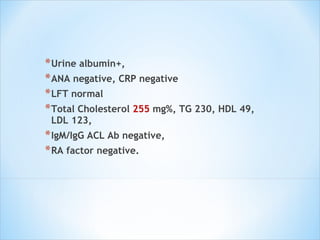
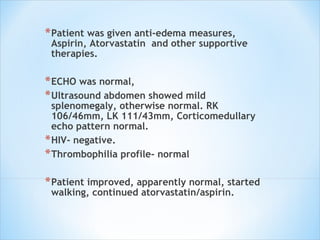
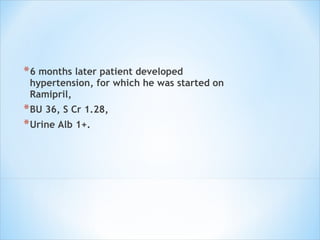
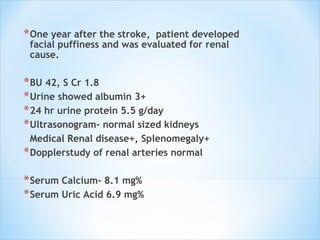
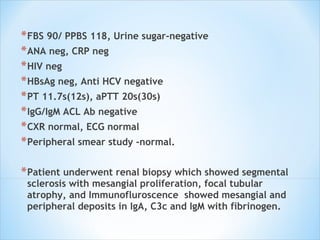
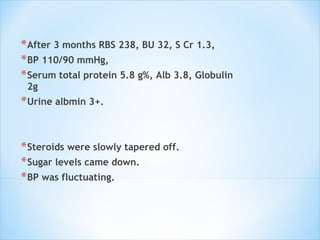
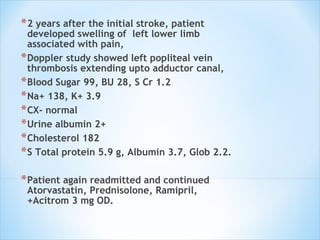
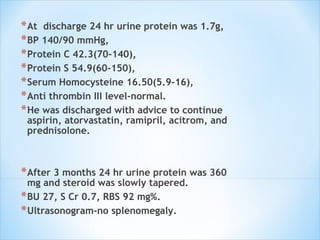
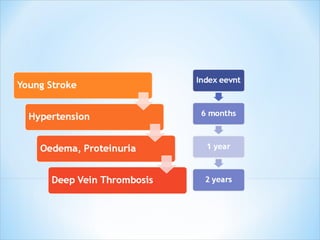
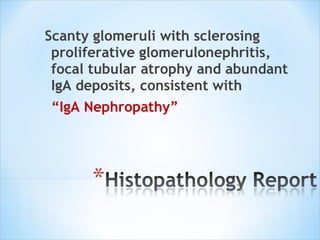
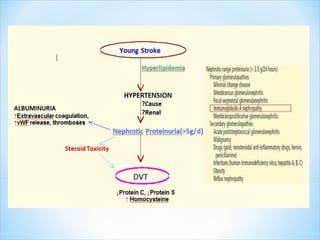
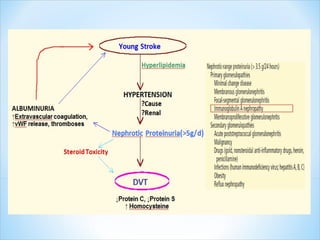
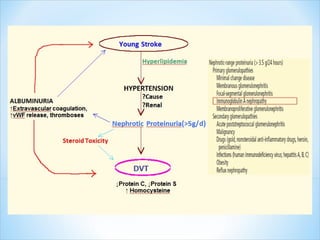
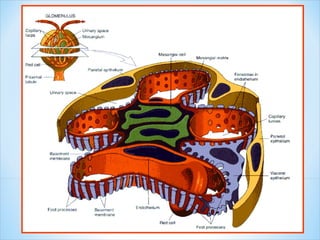
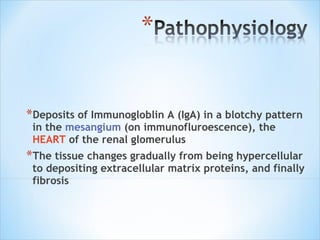
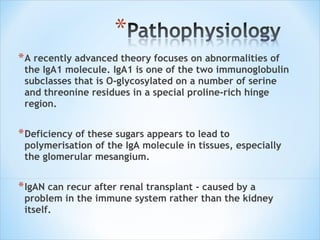
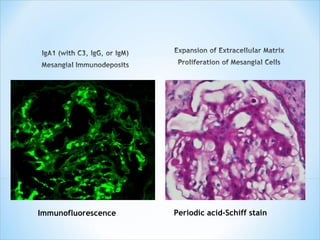
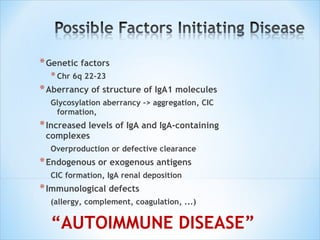
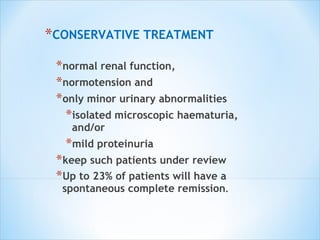
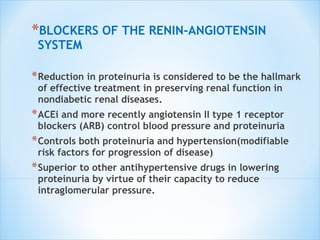
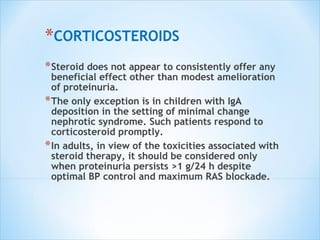
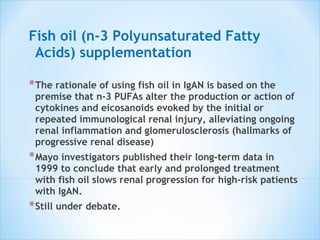
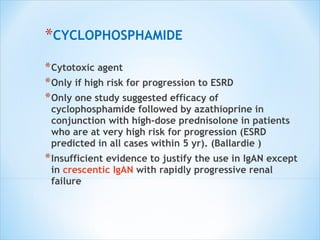
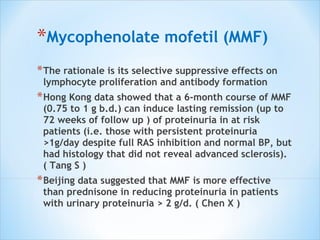
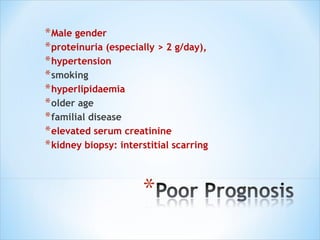
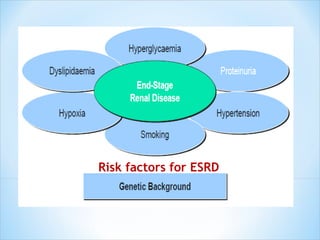
This document describes the case of a 28-year-old man who presented with inability to speak and motor weakness after fever. He was diagnosed with left middle cerebral artery territory acute infarct and a small infarct in the right parietal region. Over several years, he developed hypertension, renal dysfunction, and was ultimately diagnosed with IgA nephropathy based on renal biopsy findings. The document then provides details on IgA nephropathy including pathogenesis, histological findings, risk factors for progression, and treatment options.