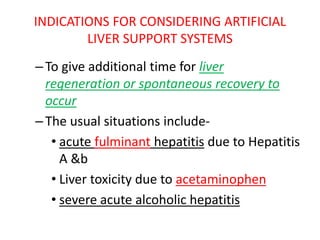
This document discusses artificial liver support systems for patients with liver failure. It begins by introducing the vital functions of the liver and describing acute and chronic liver failure. For patients awaiting transplantation or regeneration, extracorporeal devices have been developed to temporarily support liver function. Both non-cell based systems that provide detoxification and cell-based bioartificial systems that also support synthesis are described. While artificial systems have shown improvements biochemically, benefits to survival have not been clearly proven. Further development and clinical trials are still needed to establish efficacy and safety of bioartificial liver devices.