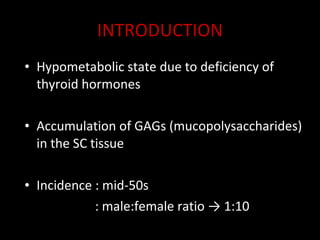
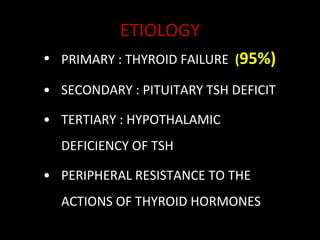
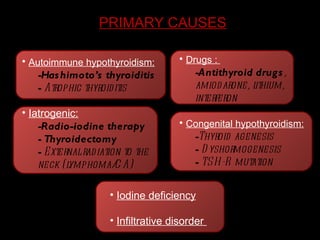
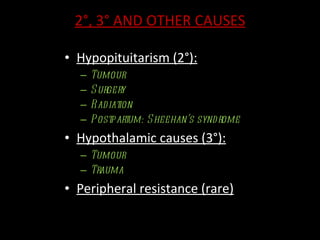
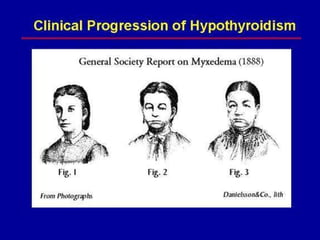
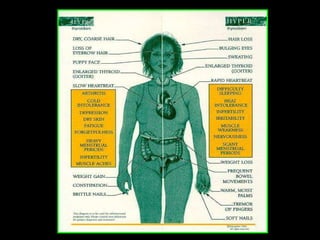
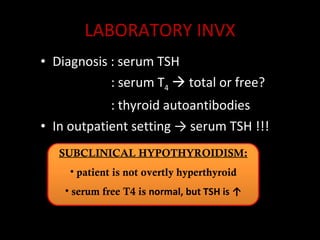
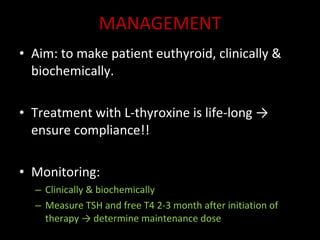
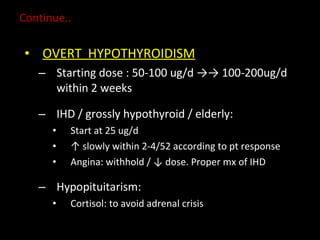
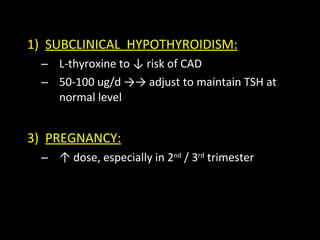
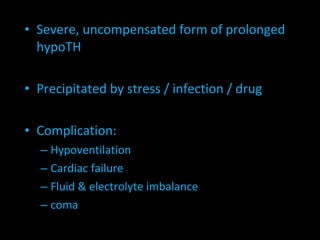
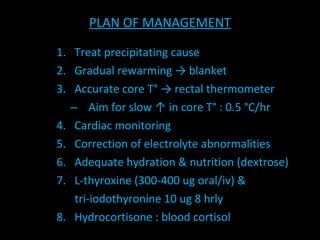
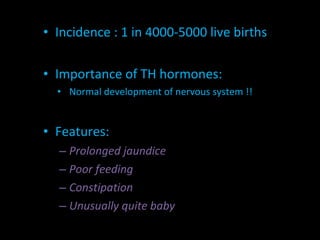
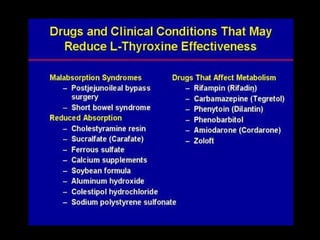
Hypothyroidism is a hypometabolic state caused by a deficiency of thyroid hormones. It can be primary, secondary, or tertiary in nature. Primary hypothyroidism is usually due to autoimmune thyroiditis or iatrogenic causes like radiation or surgery. Symptoms include fatigue, weight gain, dry skin, and constipation. Treatment involves lifelong thyroid hormone replacement therapy with levothyroxine to restore euthyroidism. Monitoring includes clinical evaluation and measurement of TSH and free T4 levels.