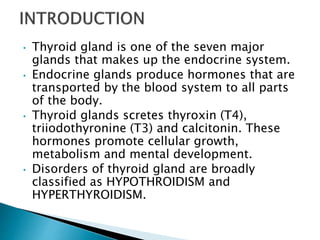
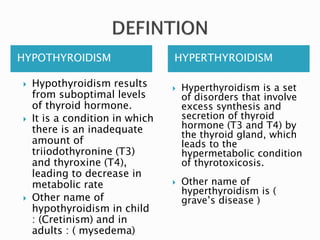
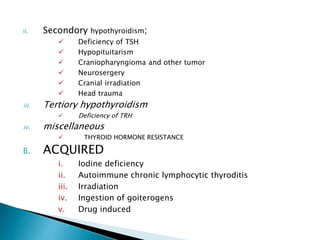
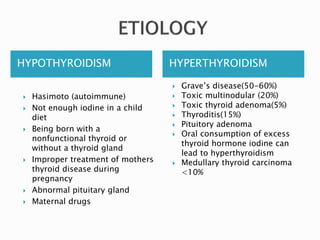
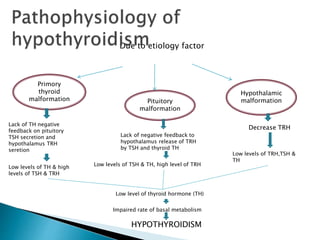
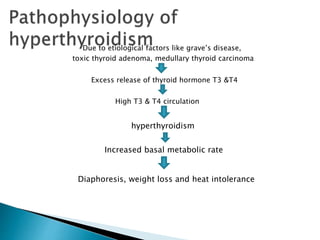
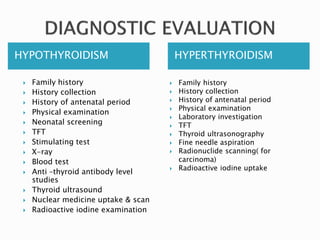
The document discusses hypothyroidism and hyperthyroidism, detailing their causes, effects, and treatment options. Hypothyroidism involves insufficient thyroid hormone leading to low metabolic rates, while hyperthyroidism results from excess hormone production causing hypermetabolic conditions. Various diagnostic and therapeutic approaches, including hormone replacement therapy and antithyroid medications, are explored for managing these thyroid disorders.

![HYPOTHYROIDISM HYPERTHYROIDISM
1. levothyroxine: 10 to 15 mcg/kg orally
once day, must be started immediately
& be closely monitored.
this dosages is intended to rapidaly
within (2week) bring the serumT4 level
into the upper half of normal range for
age ( between 10 mcg/dl [129nmol/l]
and 15mcg/dl [193nmol/l] and
promptly ( within 4 week) reduce the
TSH.
2. In acquired hypothyroidism :
usual starting dosages of
levothyroxine is based on body
surface area (100mcg/m2 orally once
a day)
For age 1 to 3 years : 4 to 6 mcg/kg once a
day
For age 3 to 10 years : 3 to 5 mcg/kg once a
day
1. Antithyroid drugs :
propylthiouracil:
6 year child ; 50mg orally daily in
3 equally divided doses
approximately
( carefully titrate based on TSH &
free T4 levels)
6 to 10 year of age ;
50 to 150 mg orally 8 hr.
10 years or older; 150 to 300 mg
orally
Methimazole ;
0.17 to 0.33 mg/kg orally 3
times a day
2. Beta blocker:
Propranolol – 0.8 mg/kg
orally 3 times a day
Atenolol- 0.5-1.2 mg/kg
orally 1 to 2 times a day](https://image.slidesharecdn.com/hyperthyroidismhypothyroidism-230505150547-d94252ac/85/hyperthyroidism-hypothyroidism-14-320.jpg)