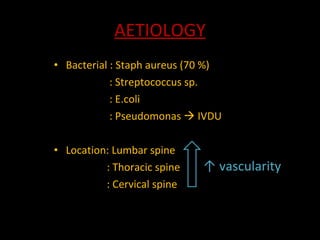
The document discusses spine infections, including pyogenic (bacterial) spine infections and non-pyogenic tuberculosis spine infections. Pyogenic infections are usually caused by Staphylococcus aureus and can spread hematogenously, presenting with back pain and fever. Diagnosis involves blood tests, imaging like CT/MRI, and treatment consists of antibiotics and possible surgery. Tuberculosis spine infections typically involve the thoracic vertebrae and can cause angular deformities. They present with chronic back pain and exposure risk factors and are treated with anti-TB drugs.