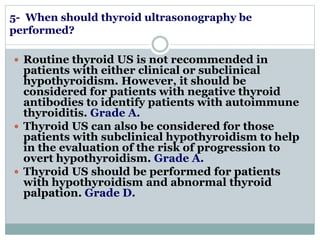
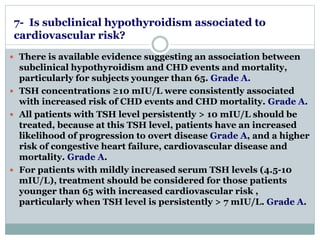
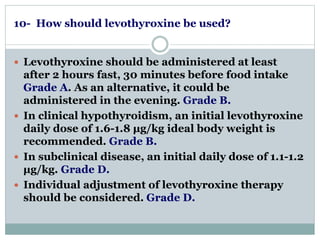
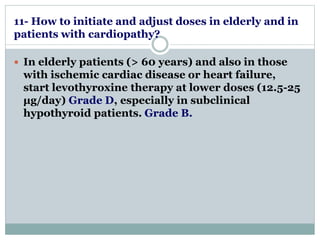
This document provides evidence-based guideline recommendations for diagnosing, screening, treating, monitoring treatment, and following up on hypothyroidism. It discusses recommendations for diagnosing hypothyroidism through TSH testing, screening high-risk groups but not asymptomatic adults, and treating with levothyroxine. It also provides guidance on monitoring treatment through periodic TSH testing, adjusting doses for elderly patients and those with heart conditions, and addressing persistent symptoms or high TSH levels despite treatment.