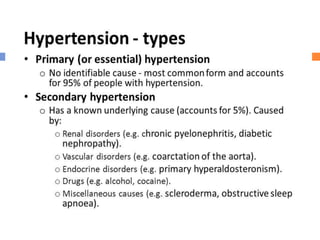
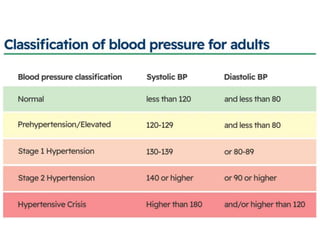
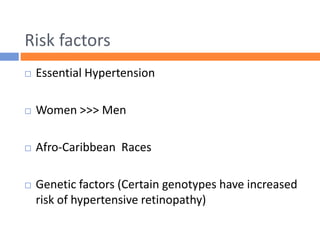
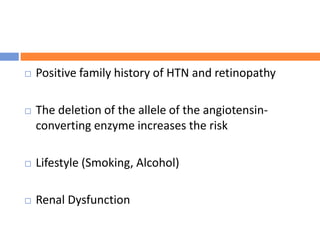
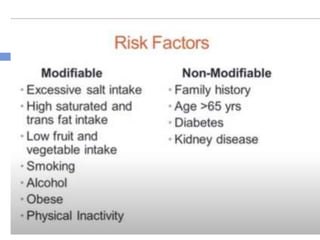
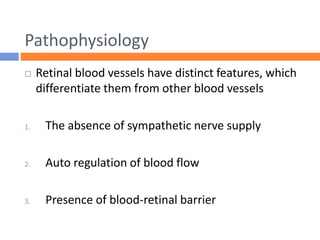
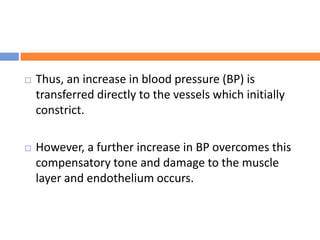
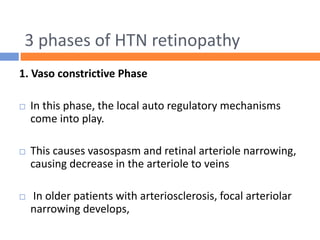
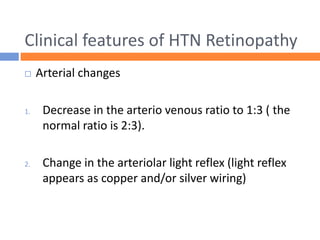
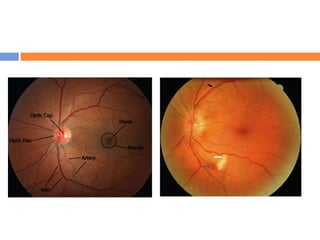
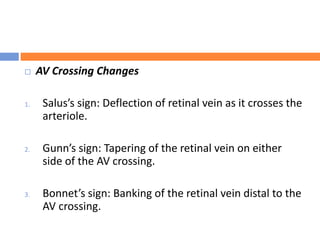
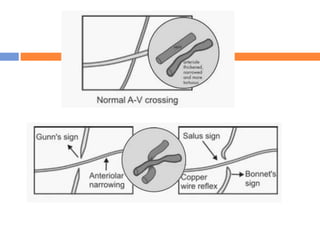
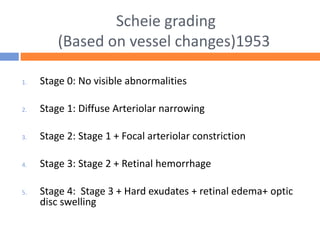
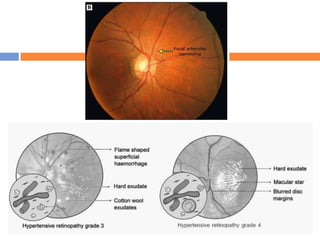
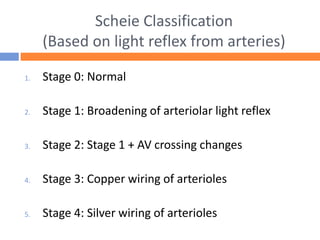
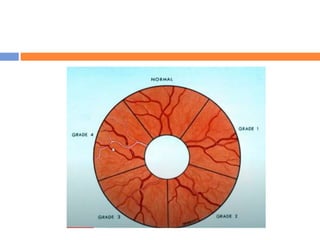
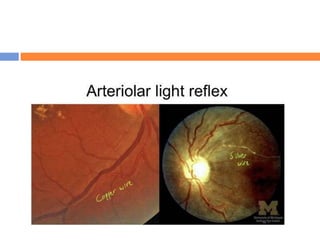
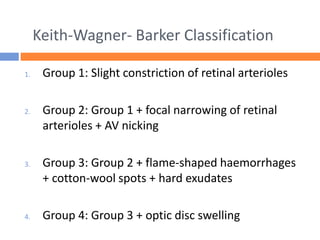
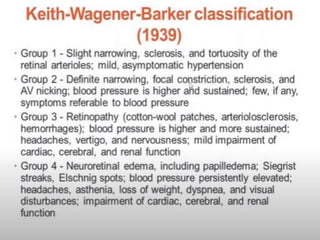
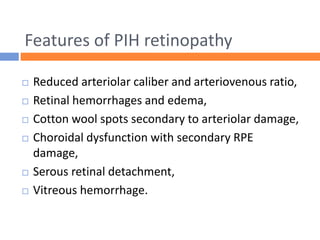
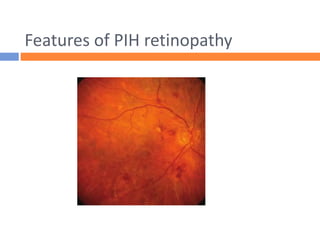
This document summarizes hypertensive retinopathy, which occurs when retinal vessels are damaged due to elevated blood pressure. It discusses the types and clinical features of hypertensive retinopathy, including changes to retinal arteries and veins seen on examination. It also covers classifications of hypertensive retinopathy based on vessel changes and light reflexes. Risk factors, pathophysiology, and complications are described. Treatment involves controlling blood pressure through lifestyle changes and medication. Uncontrolled high blood pressure can lead to further eye and systemic damage.

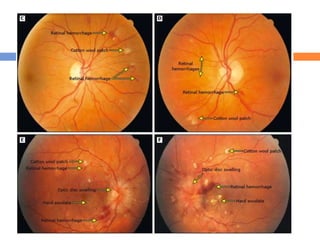
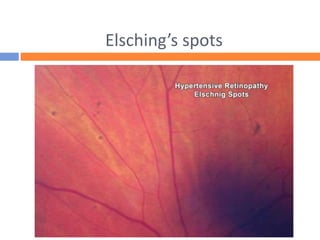
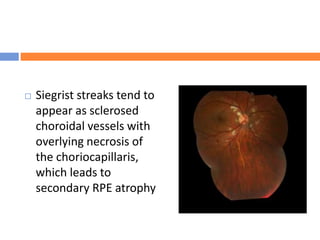
![ Malignant hypertension can also cause choroidopathy.
Fibrinoid necrosis of choroidal arterioles leads to
segmental infarction of choriocapillaris.[10] Poor
perfusion of the choriocapillaris causes Elschnig spots,
defined as hyperpigmented patches in the choroid
surrounded by a ring of hypopigmentation, or Siegrist
streaks, defined as linear hyperpigmented lesions over
choroidal arteries. Hypertensive choroidopathy can
cause a focal pigment epithelium detachment, leading
to exudative retinal detachment.[4] Generally,
hypertensive choroidopathy affects younger patients
with malignant hypertension.[13]](https://image.slidesharecdn.com/htnretinopathy-221202084656-5a04928f/85/HYPERTENSIVE-RETINOPATHY-pptx-57-320.jpg)