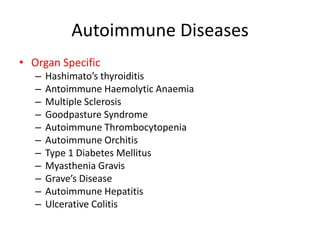
Autoimmunity occurs when the immune system fails to recognize self antigens and mounts an immune response against the body's own cells and tissues, leading to autoimmune disease. The immune system normally develops tolerance through central and peripheral mechanisms to distinguish self from non-self. A breakdown in tolerance can result from genetic susceptibility and environmental triggers like infections that cause molecular mimicry or tissue damage releasing self antigens. Autoimmune diseases are classified as organ-specific if they target a single organ, or systemic if affecting multiple body systems.