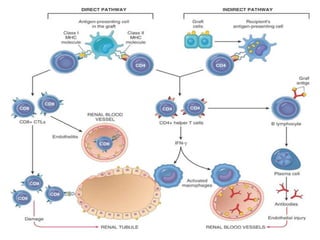
Rejection is a complex process where the recipient's immune system attacks the transplanted organ or graft as foreign. It involves both cell-mediated and antibody-mediated immunity. There are three main types of rejection: hyperacute rejection which occurs within minutes/hours due to pre-existing antibodies, acute rejection within months due to an immune response, and chronic rejection over longer periods due to inflammation. Preventing rejection requires immunosuppressive drugs or techniques to block co-stimulatory signals needed for an immune response.