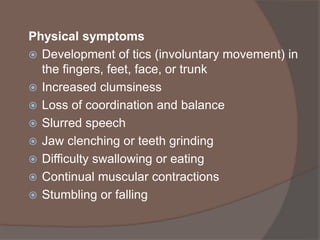
Huntington's disease is a hereditary, progressive brain disorder causing physical, mental, and emotional changes, primarily affecting the basal ganglia and cortex. Diagnosis involves genetic testing and clinical evaluation, while symptoms include cognitive decline, mood changes, and involuntary movements, typically starting between ages 30-50. There is currently no cure, and treatment focuses on managing symptoms and improving quality of life through a multi-disciplinary approach.