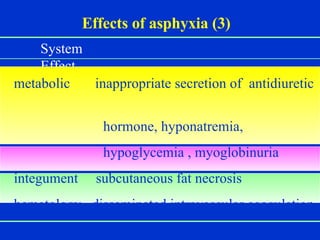
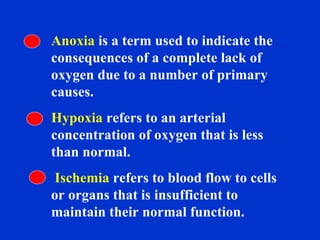
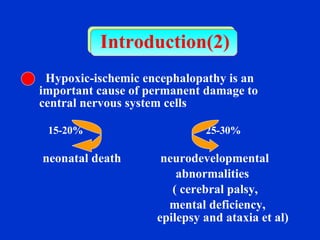
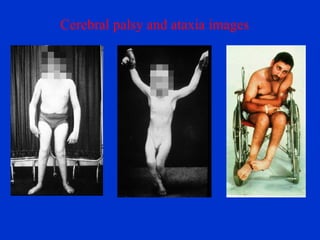
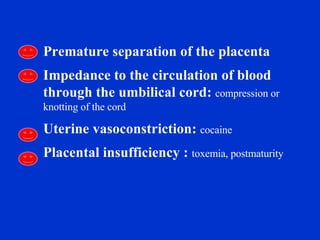
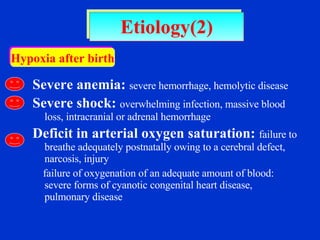
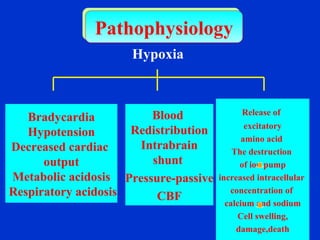
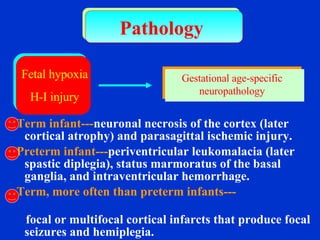
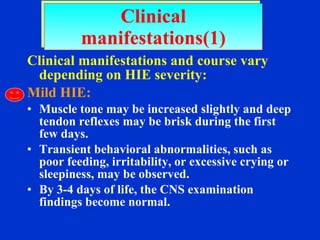
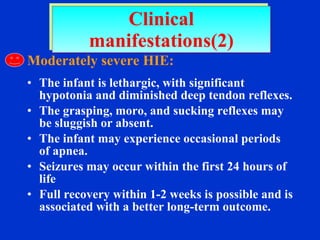
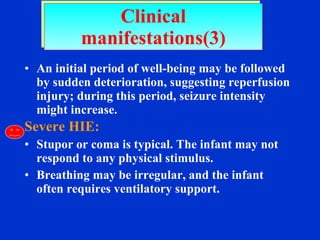
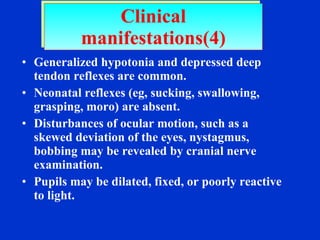
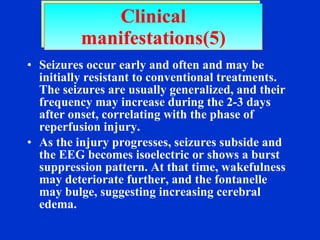
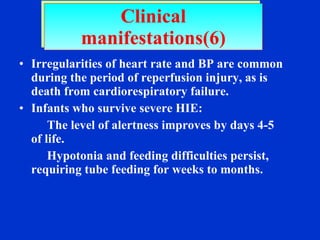
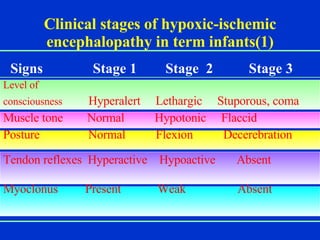
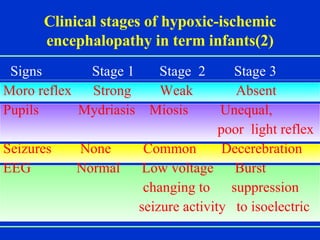
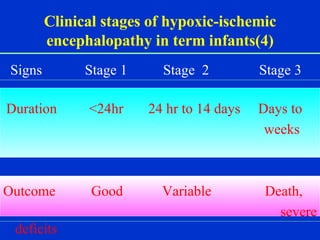
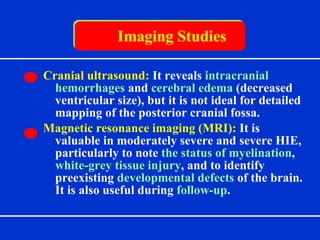
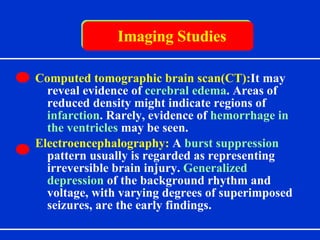
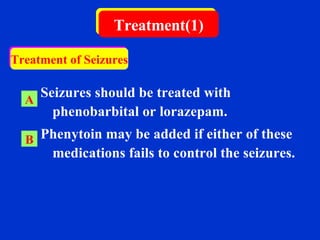
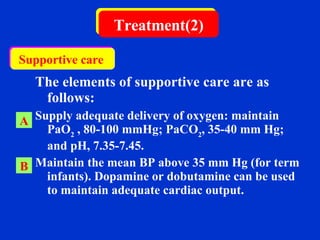
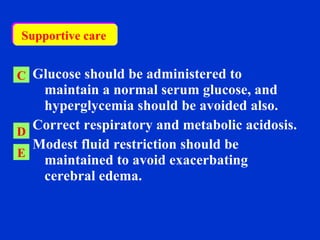
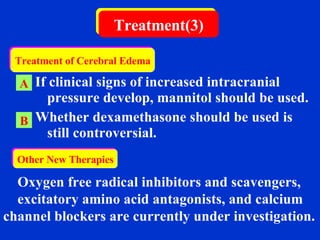
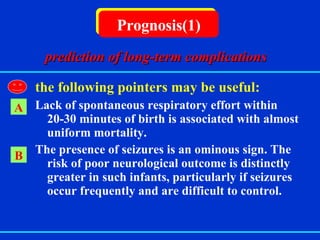
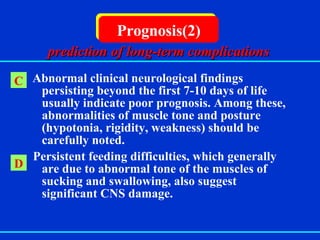
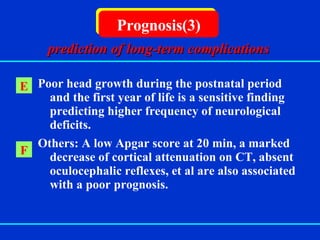
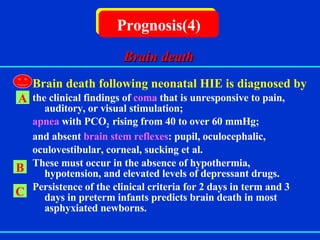
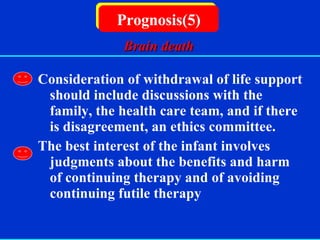
Neonatal hypoxic-ischemic encephalopathy (HIE) occurs when the brain is damaged due to a lack of oxygen before, during, or after birth. It can cause long-term complications such as cerebral palsy, intellectual disability, epilepsy, or death. The document discusses the causes, clinical presentation, treatment, and prognosis of HIE, noting that outcomes depend on the severity of the brain injury and may include permanent neurological deficits or death. Imaging studies and supportive care aim to prevent further brain damage while treatments for seizures and cerebral edema can help reduce complications. Factors like abnormal clinical findings persisting over a week suggest a poor prognosis.