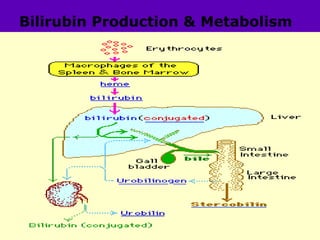
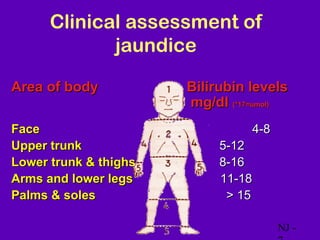
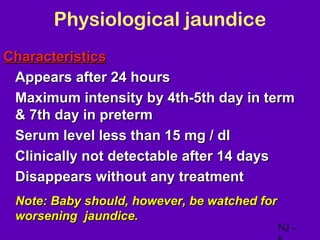
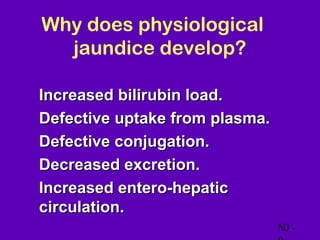
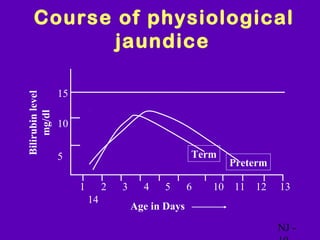
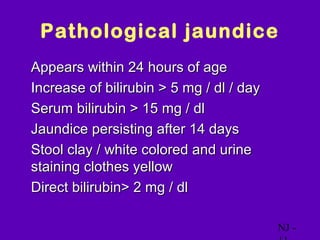
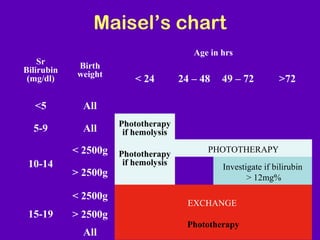
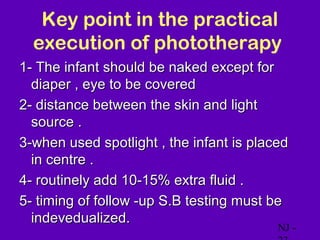
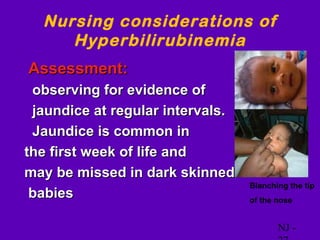
This document discusses neonatal jaundice (hyperbilirubinemia), which presents as yellowing of the skin in newborns. It defines jaundice and differentiates between physiological and pathological types. Causes of jaundice include hemolytic diseases, infections, and metabolic disorders. The main treatment is phototherapy to reduce bilirubin levels. Nursing considerations involve regular assessment of jaundice and hydration during phototherapy to prevent complications like dehydration and skin damage. The goals are to appropriately treat high bilirubin levels while avoiding therapy side effects and supporting the family.