This document summarizes the history and mechanisms of jaundice and kernicterus. Some key points include:
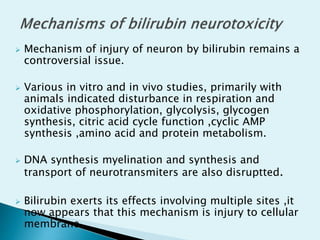
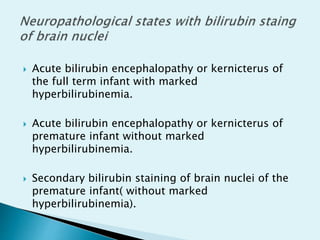
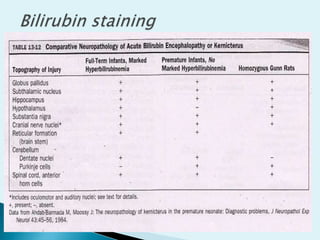
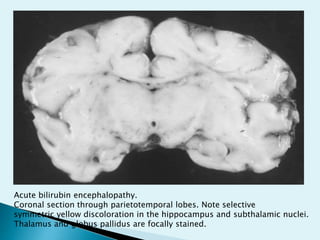
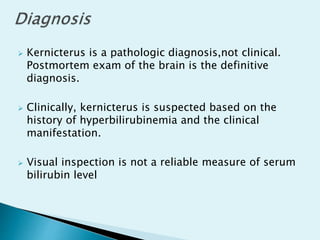
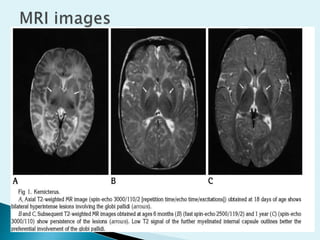
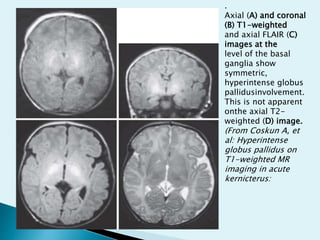
- Kernicterus was first described in 1875 and results from bilirubin accumulation in the brain due to hyperbilirubinemia.
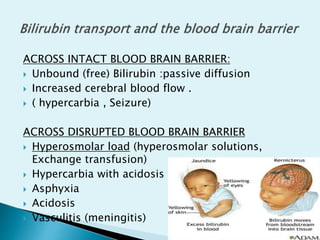
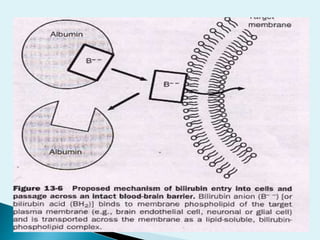
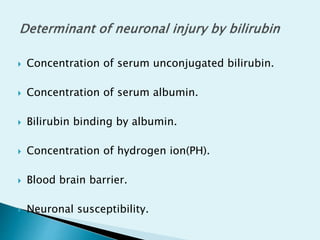
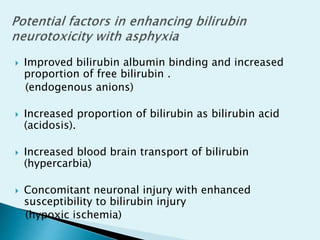
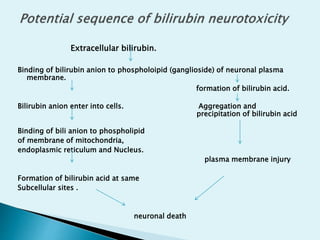
- Bilirubin exists in two forms - a water-soluble dianion and insoluble bilirubin acid. The acid form can cross the blood brain barrier.
- Two transporters, MRPs and MDR/PGP, help prevent bilirubin entry into the brain from the blood under normal conditions.
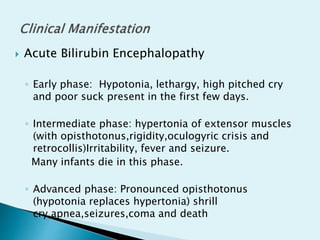
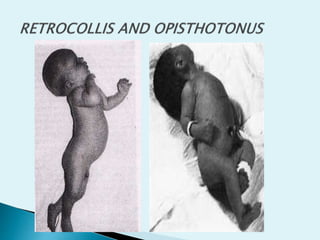
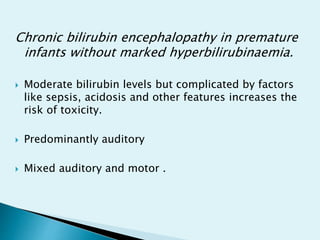
- Kernicterus presents as acute bilirubin encephalopathy with symptoms ranging