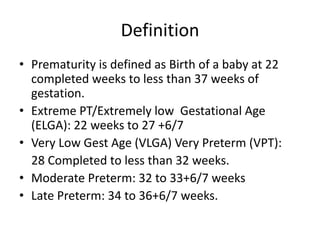
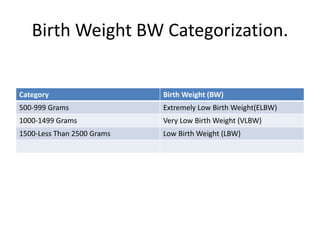
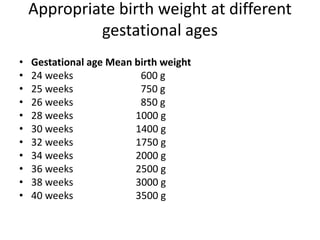
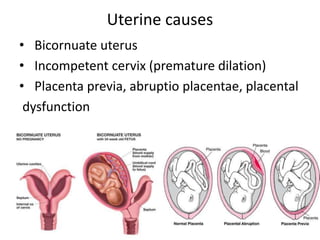
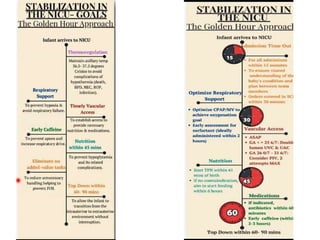
Prematurity is defined as the birth of a baby between 22 and 36 weeks of gestation, with various classifications based on birth weight and gestational age. The document discusses causes of prematurity, immediate and long-term complications, management strategies, and discharge criteria for premature infants. Key aspects of management include stabilization during the 'golden hour', maintaining a thermally neutral environment, careful monitoring of fluid and oxygen levels, and individualized feeding plans.