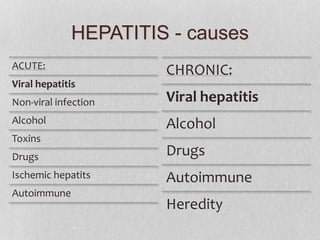
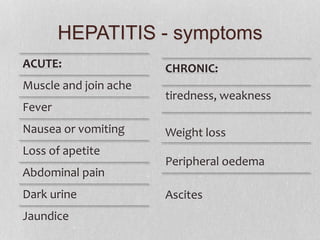
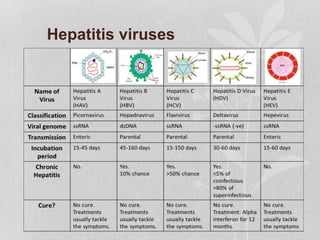
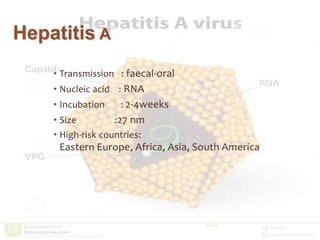
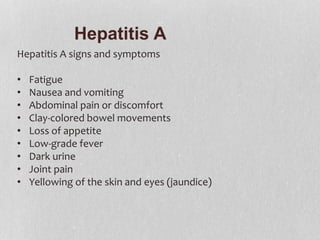
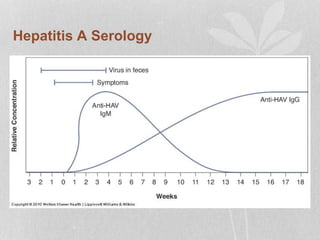
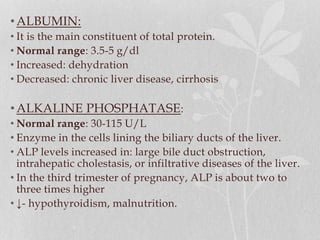
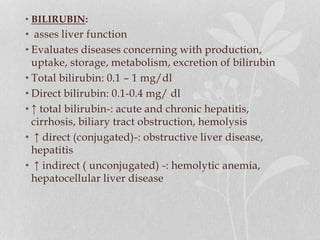
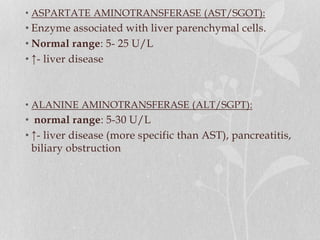
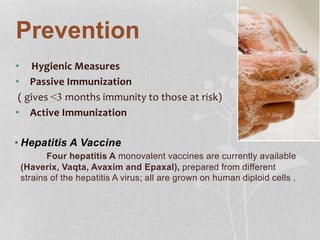
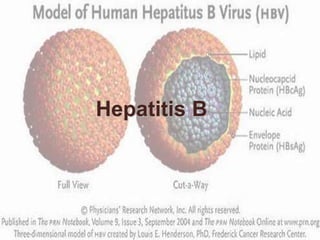
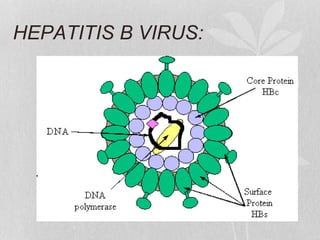
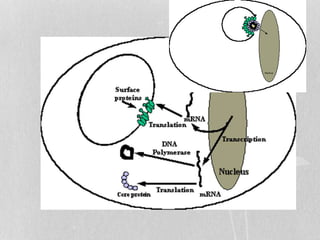
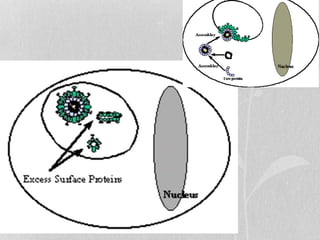
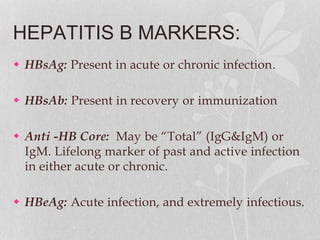
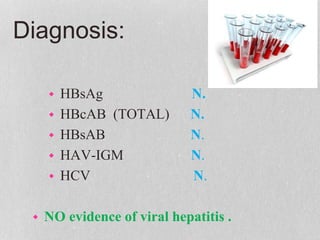
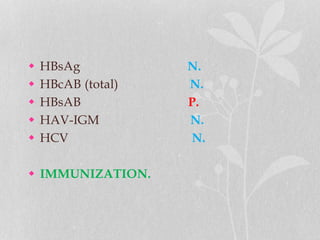
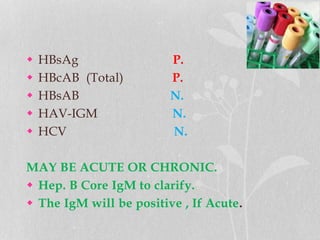
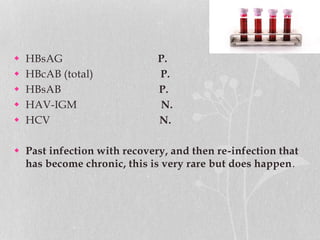
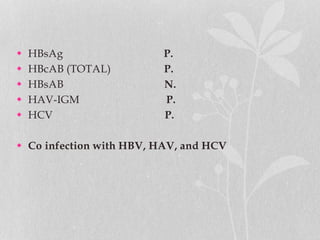
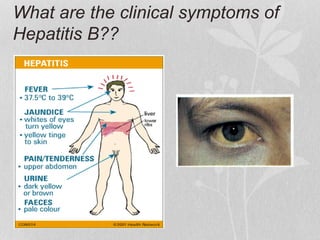
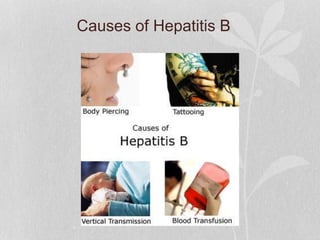
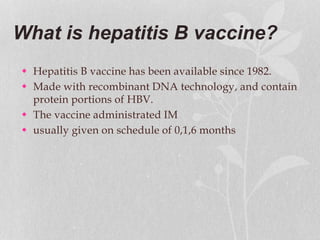
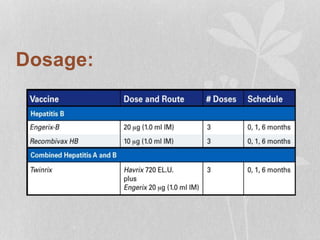
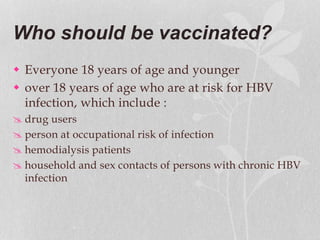
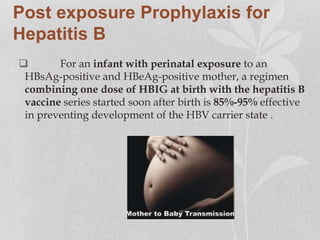
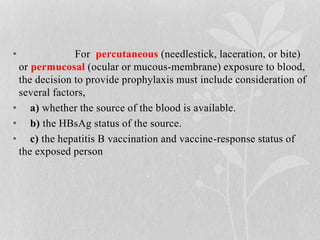
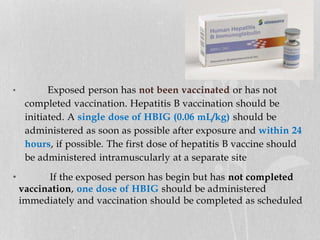
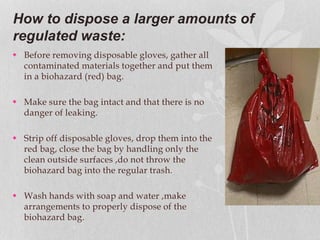
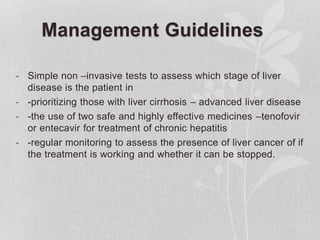
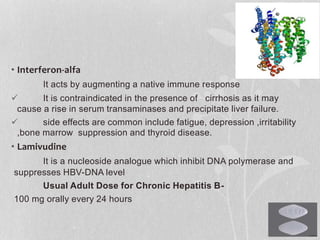
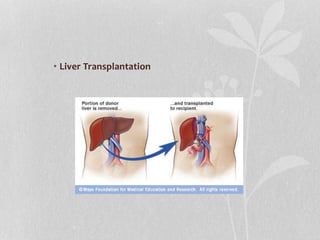
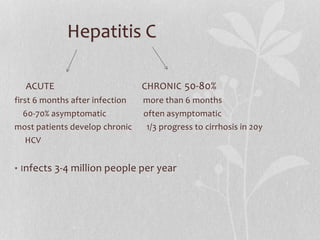
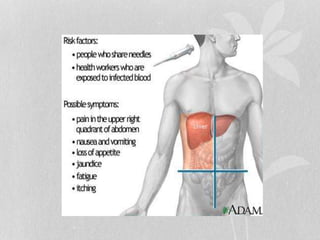
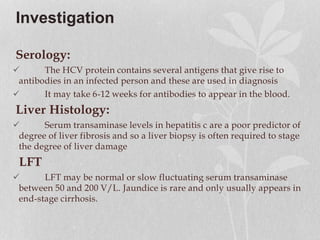
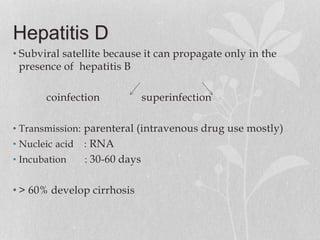
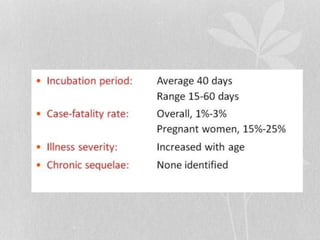
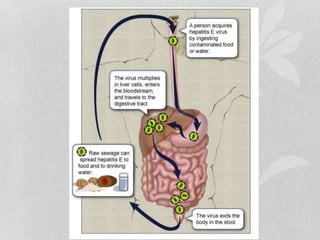
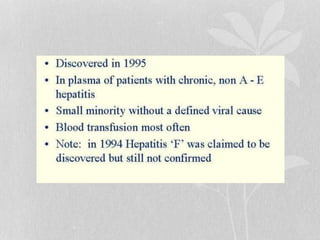
This document discusses hepatitis and its prevention. It begins with an introduction and history of hepatitis, noting its identification as an infectious disease in the 8th century. It then classifies and describes the features, symptoms, transmission, investigation and management of the main types of hepatitis - A, B, C, D and E. For hepatitis A, it outlines the faecal-oral transmission, RNA nature, incubation period and high risk countries. Prevention methods like vaccination and immune serum globulin are discussed. Hepatitis B pathogenesis, markers, diagnosis, vaccination and post-exposure prophylaxis are explained in detail. Guidelines for workplace safety practices are also provided.