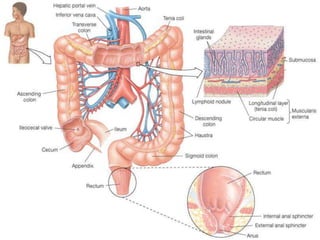
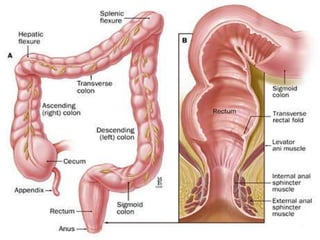
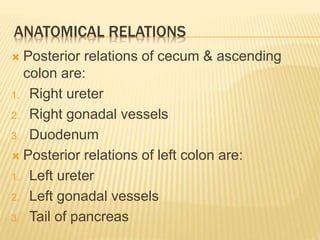
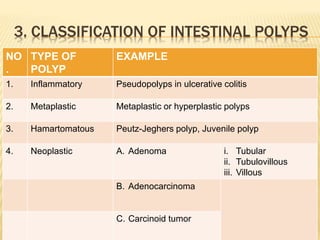
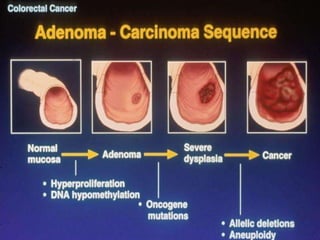
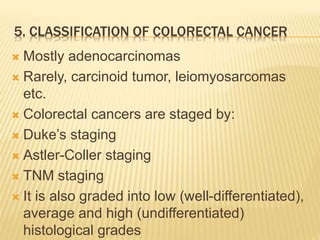
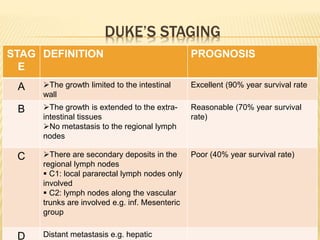
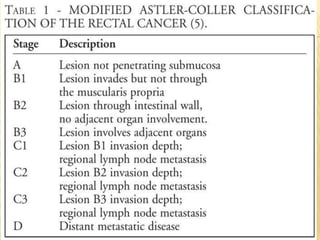
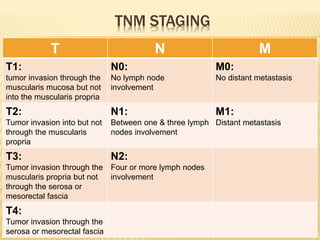
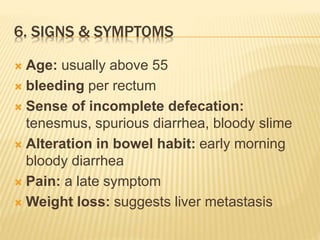
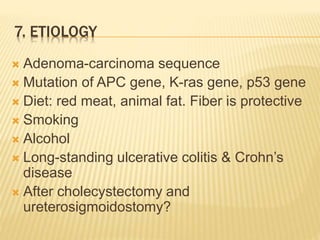
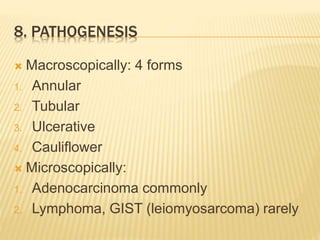
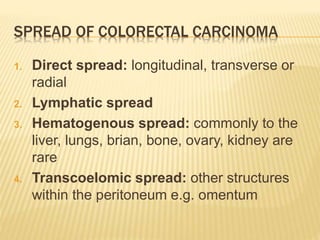
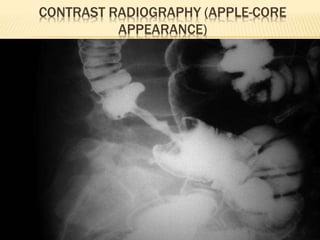
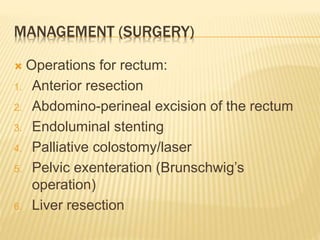
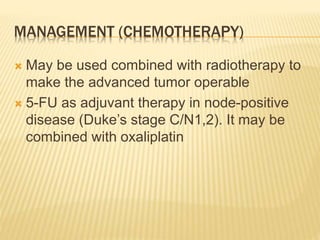
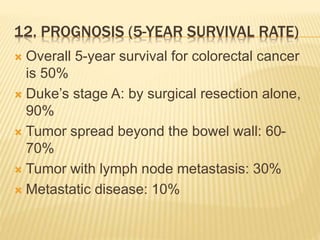
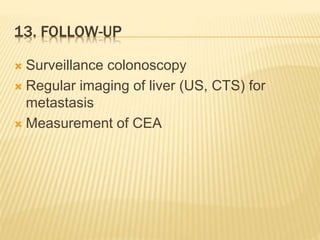
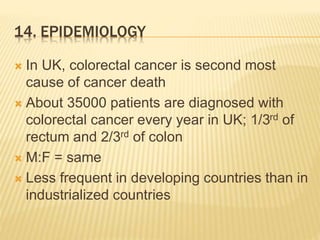
The document provides a comprehensive overview of colorectal neoplasms, covering clinical anatomy, physiology, types of polyps, cancer progression, diagnosis, prevention, and management strategies including surgery, chemotherapy, and radiation. It highlights the prevalence of colorectal cancer, particularly in the UK, and outlines important factors such as signs and symptoms, etiology, pathogenesis, and prognostic indicators related to the disease. The document is intended for a medical audience, focusing on the critical aspects of colorectal conditions and their treatment.