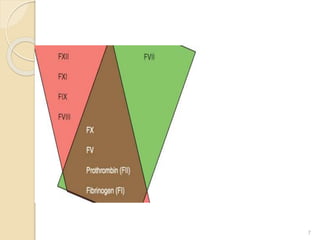
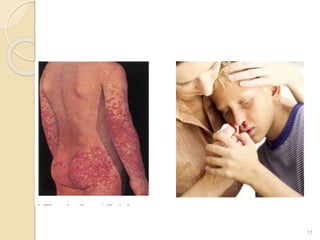
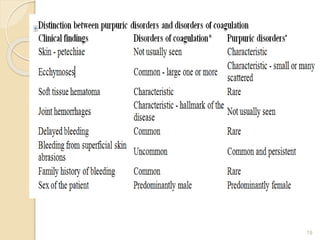
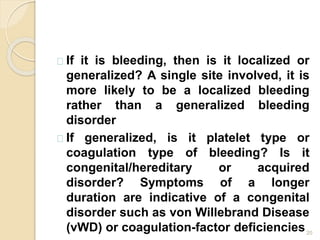
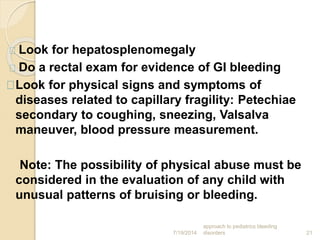
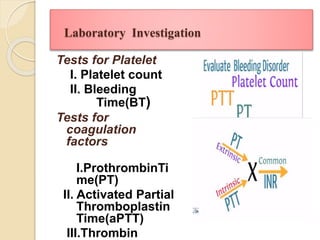
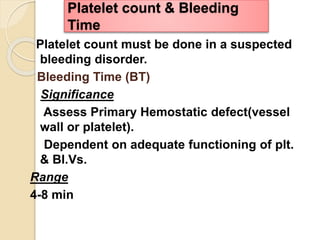
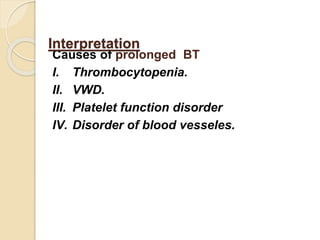
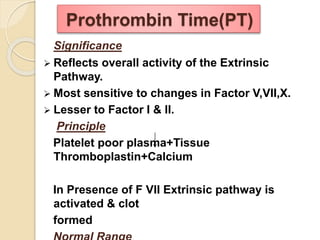
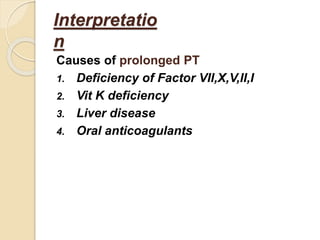
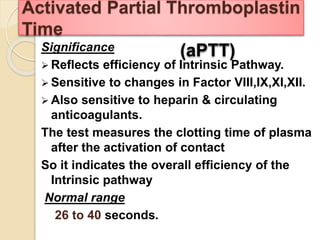
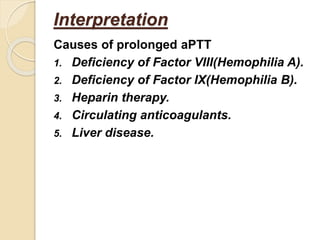
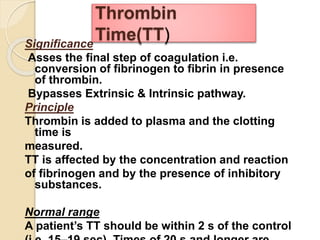
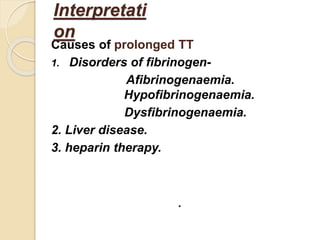
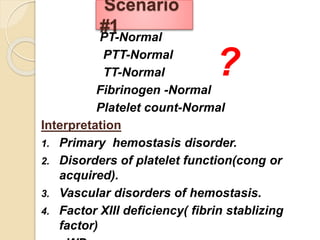
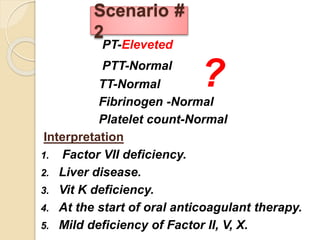
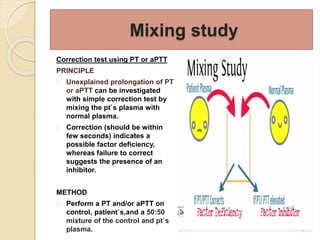
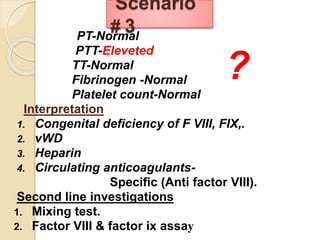
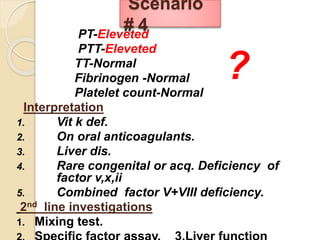
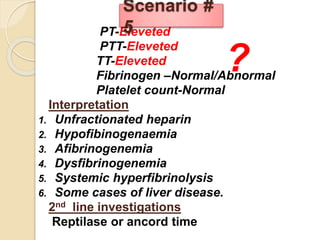
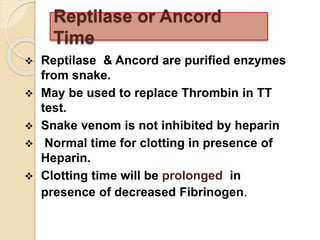
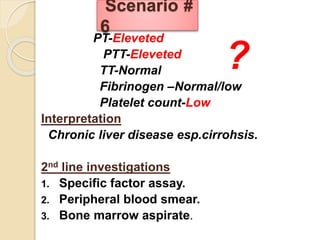
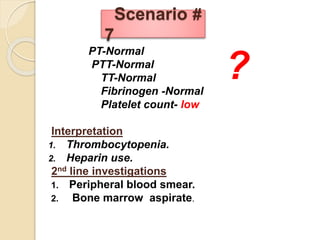
The document outlines the approach to diagnosing and managing bleeding disorders, emphasizing the importance of history taking, physical examination, and laboratory investigations. It describes the mechanisms of hemorrhage, types of bleeding disorders, and diagnostic tests for evaluating platelet and coagulation function. The document also provides detailed scenarios for interpreting laboratory findings in suspected bleeding disorders.