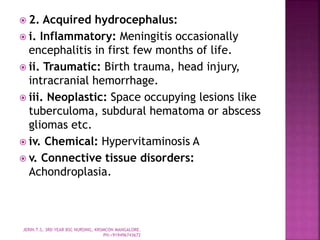
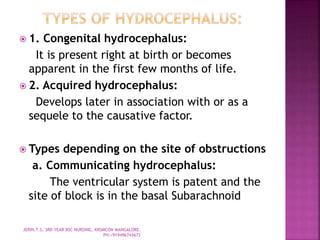
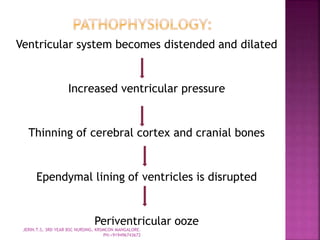
Hydrocephalus is characterized by an abnormal accumulation of cerebrospinal fluid in the brain ventricles. It can be caused by increased CSF production, decreased absorption, or blockage of CSF flow pathways. The document discusses the types, causes, signs and symptoms, diagnostic tests, treatment including shunt surgeries, and nursing management of hydrocephalus.