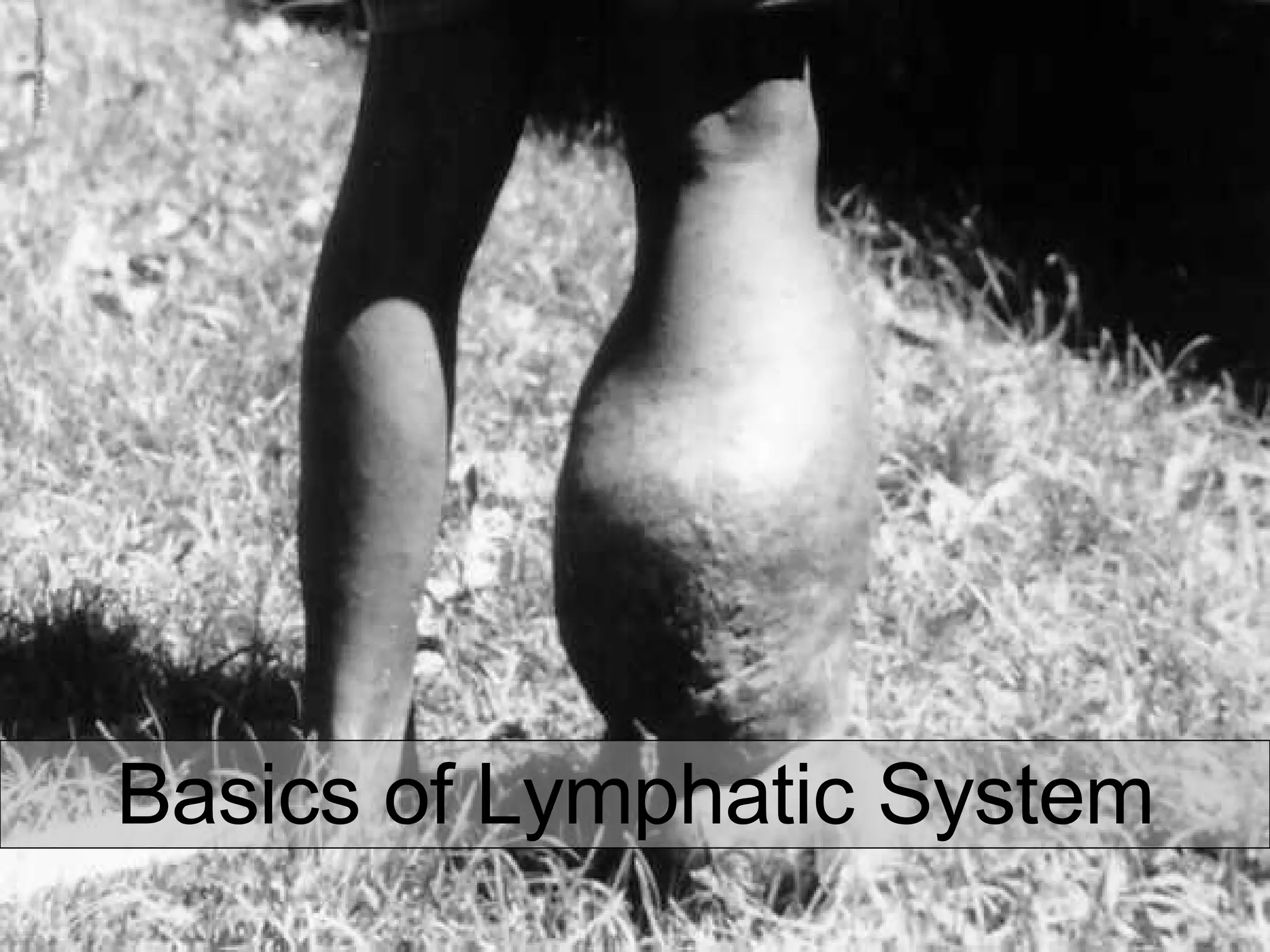
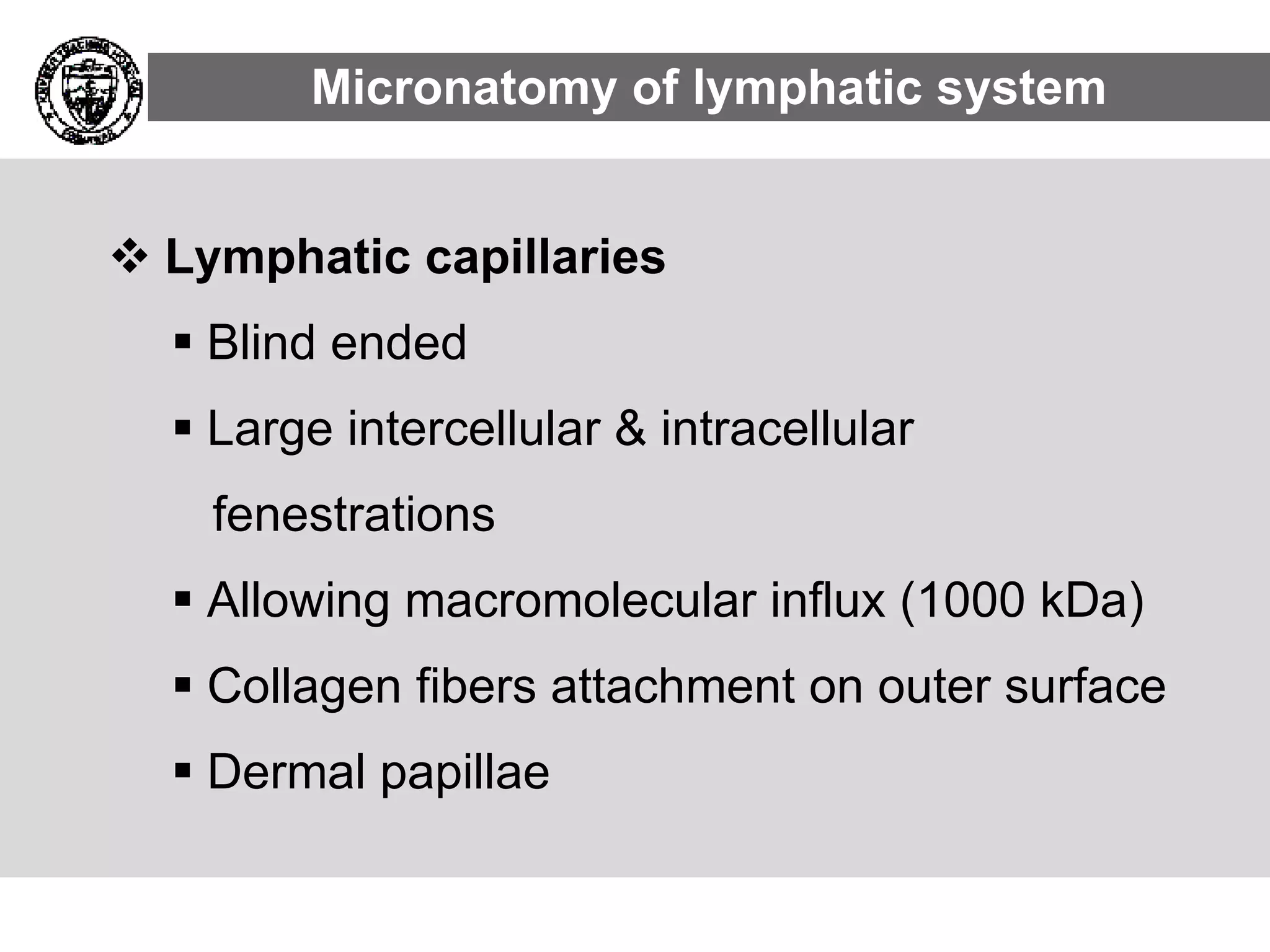
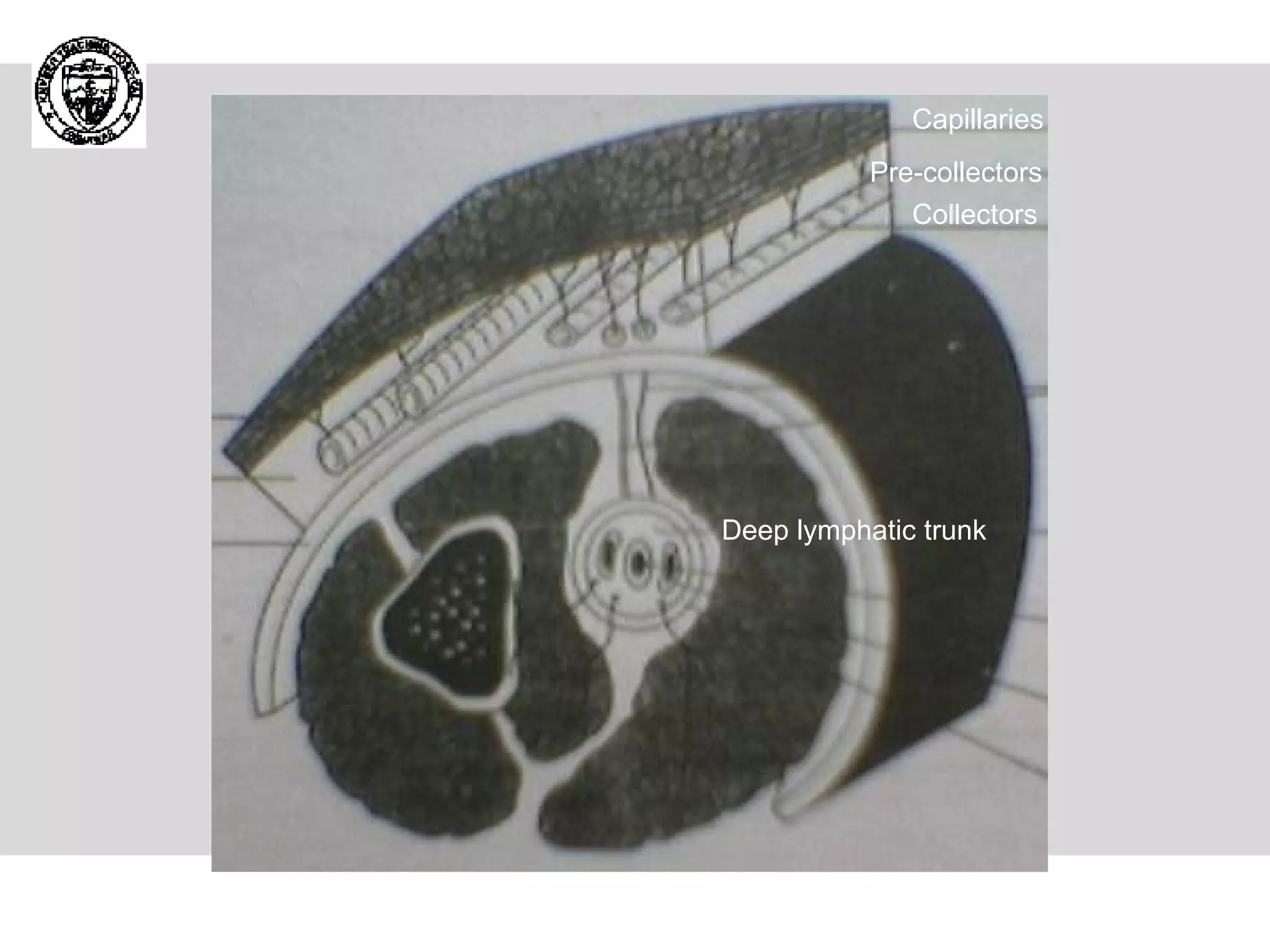
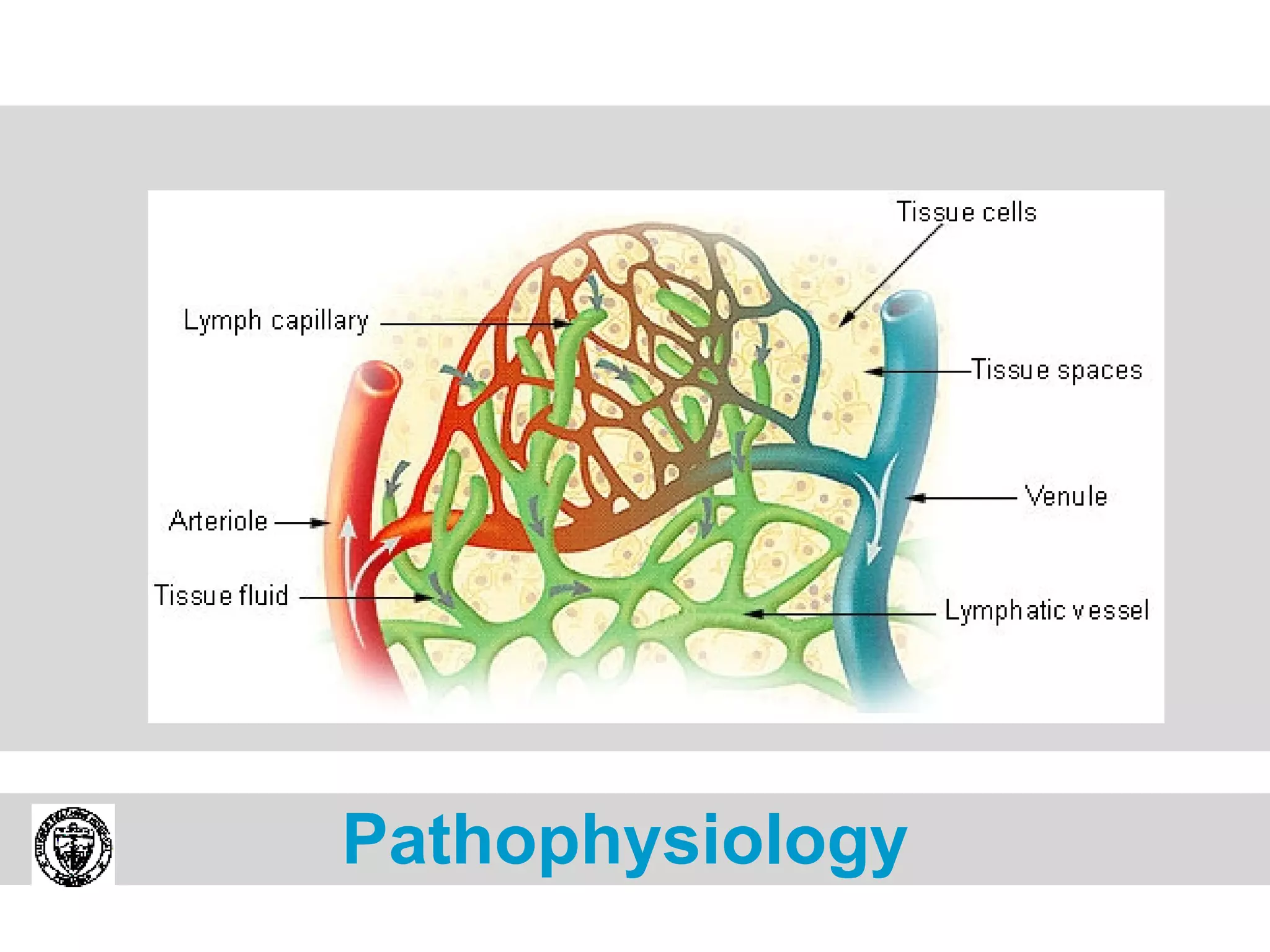
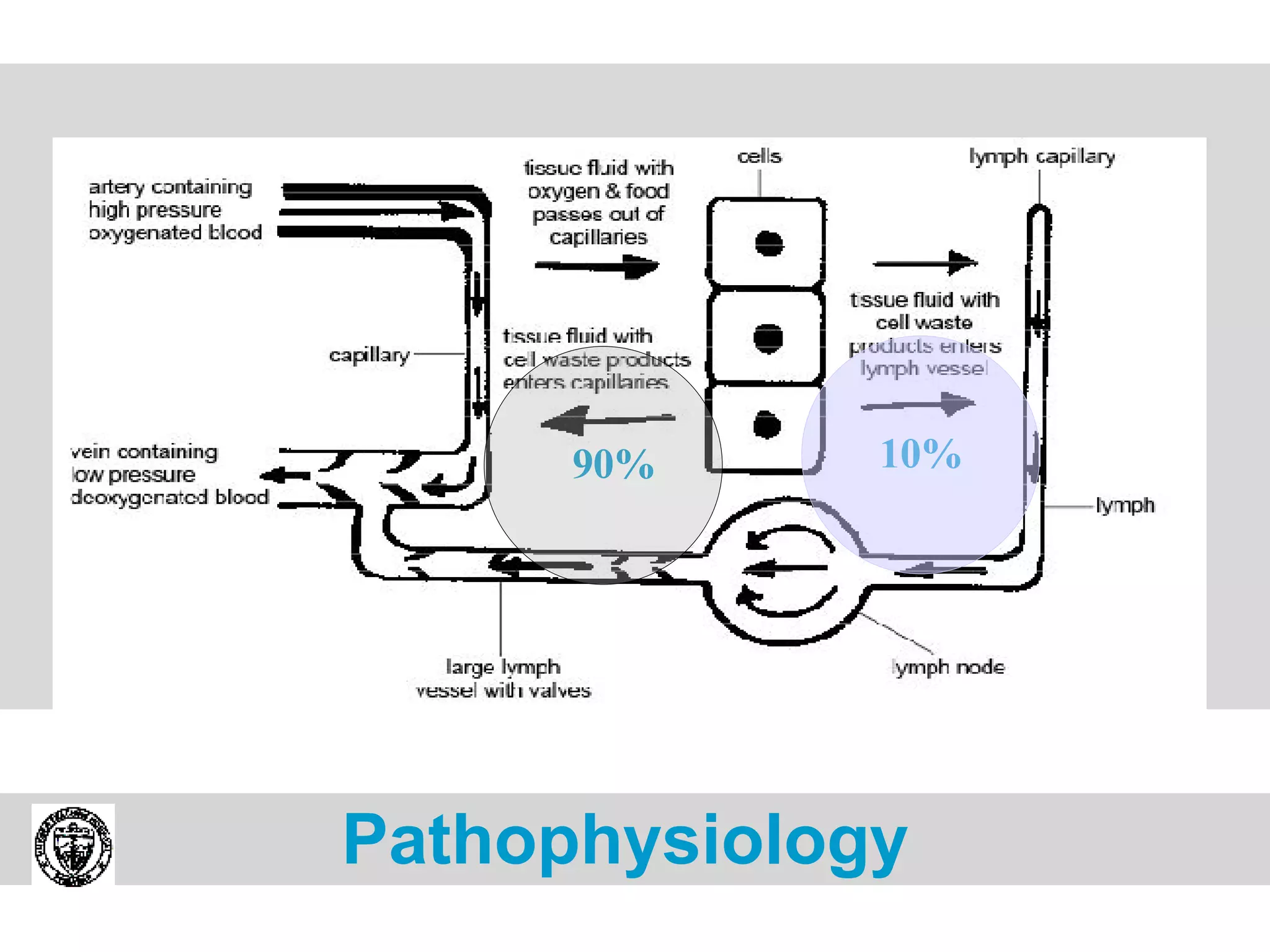
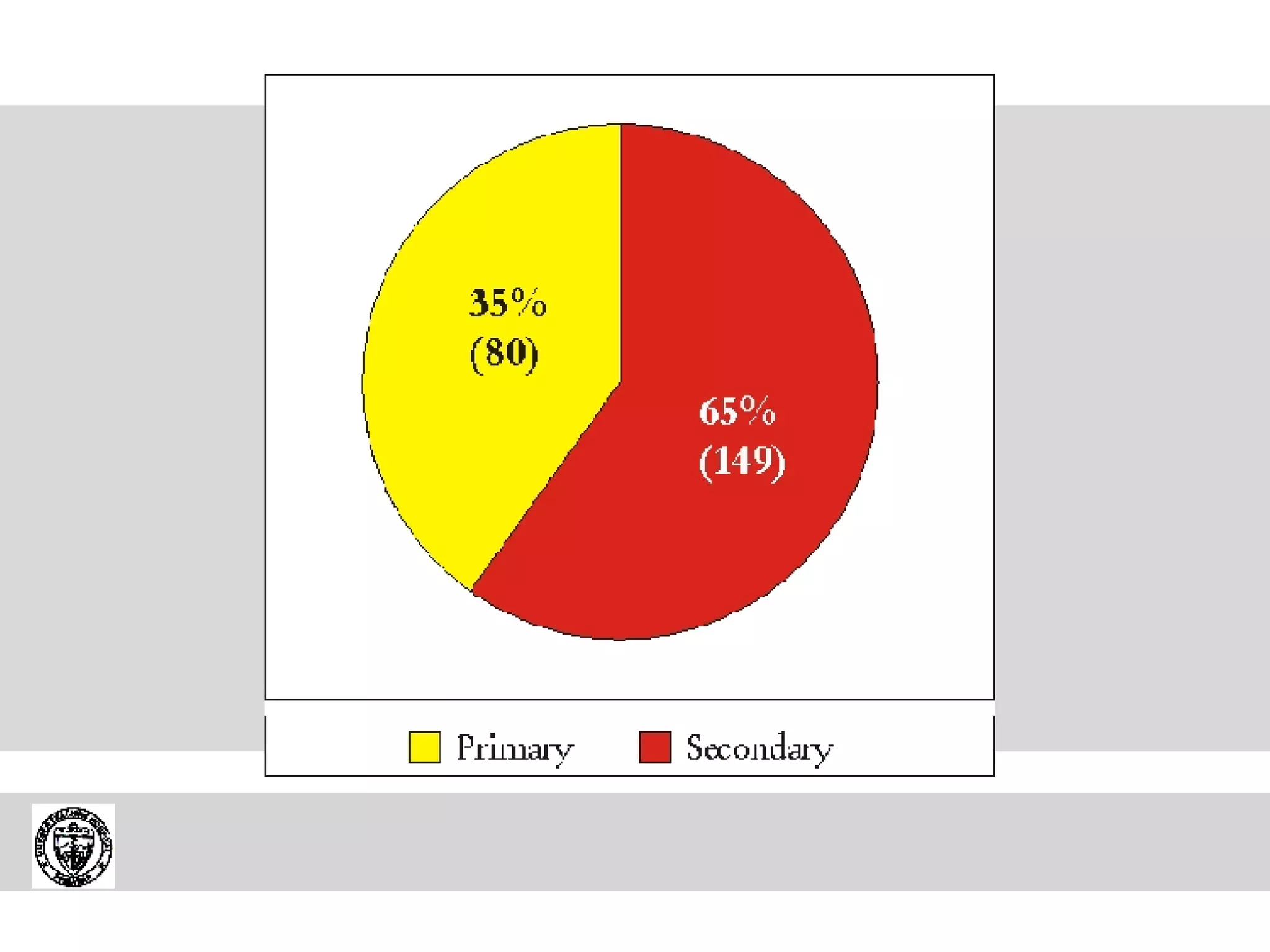
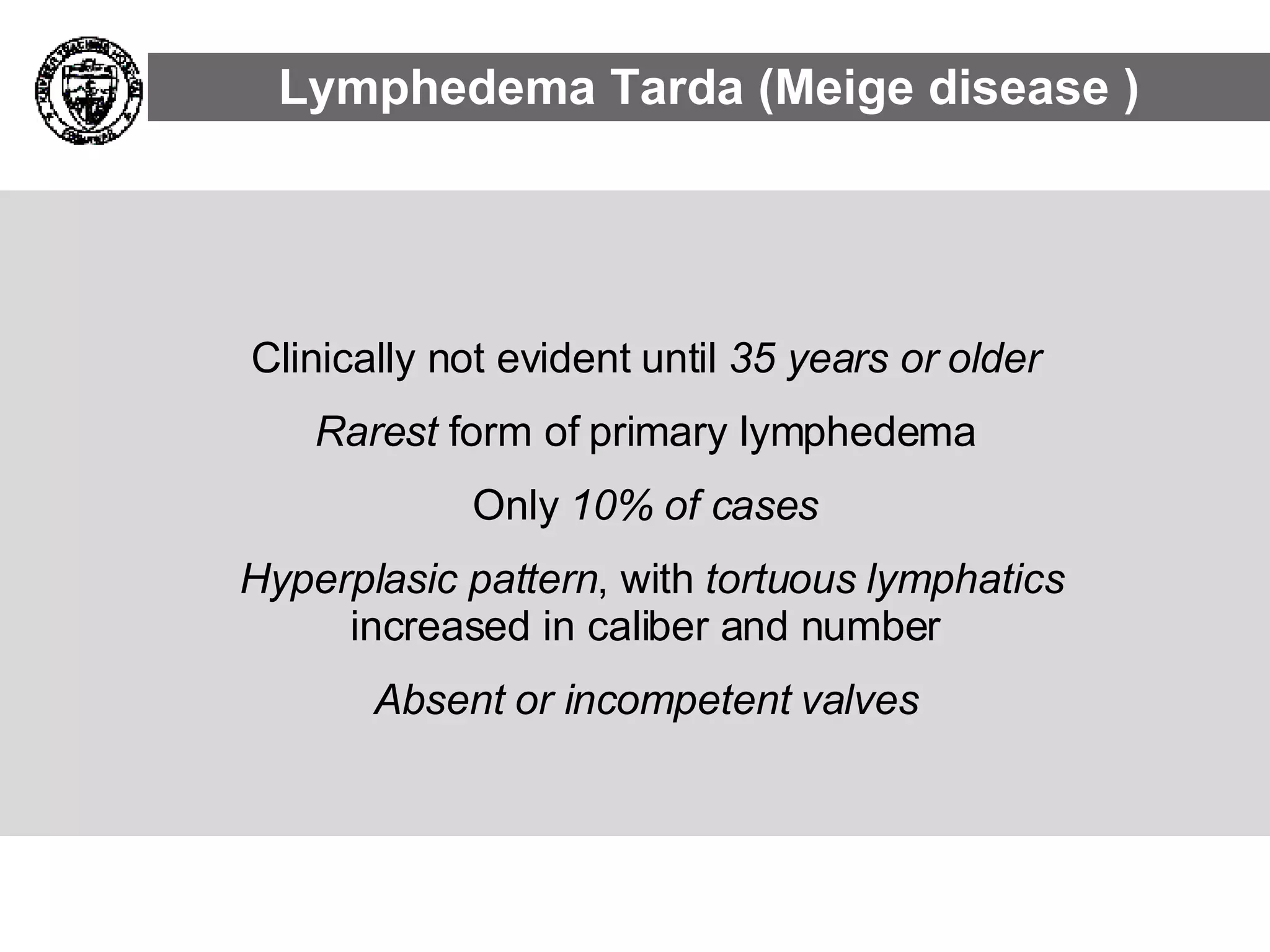
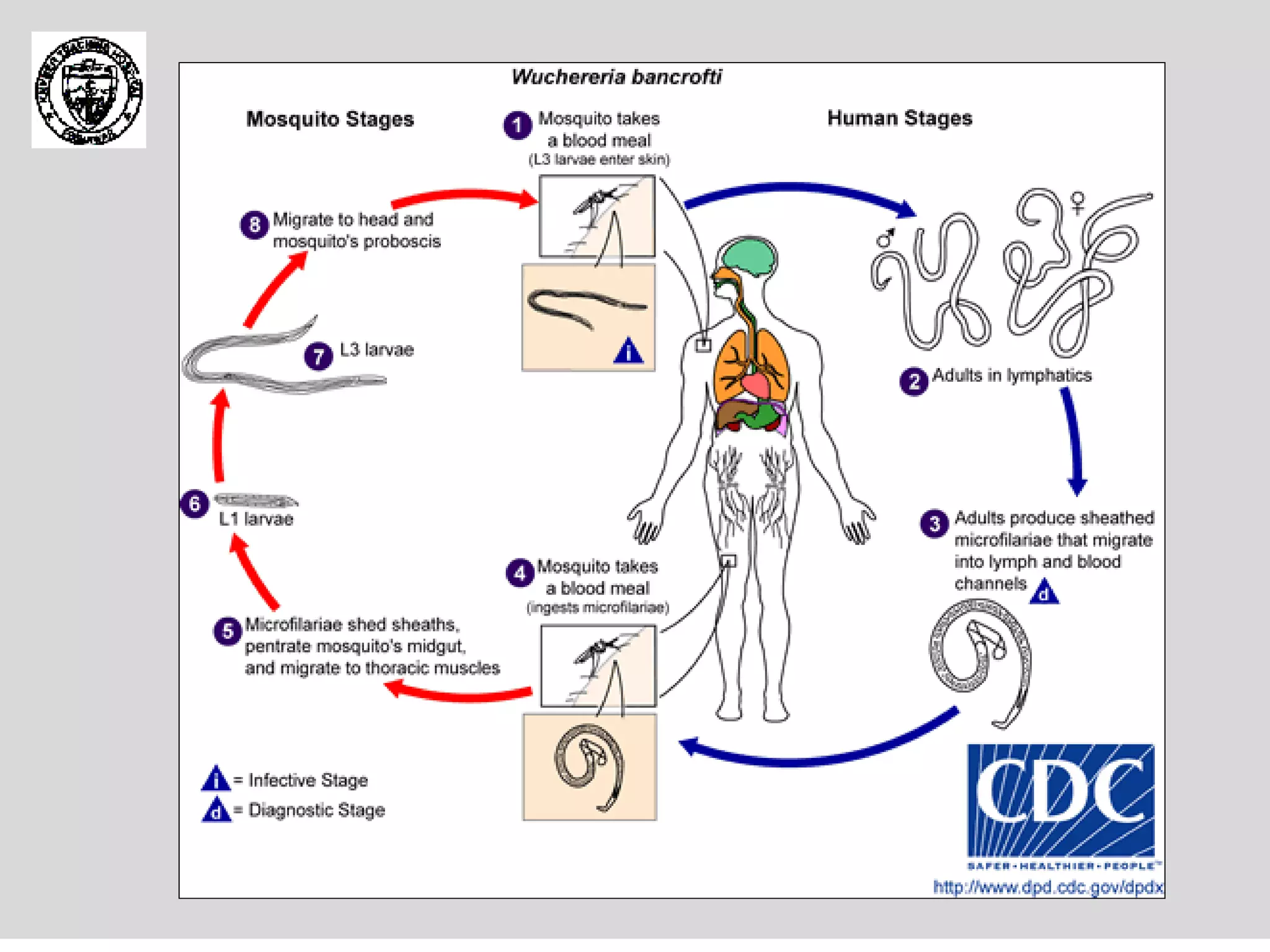
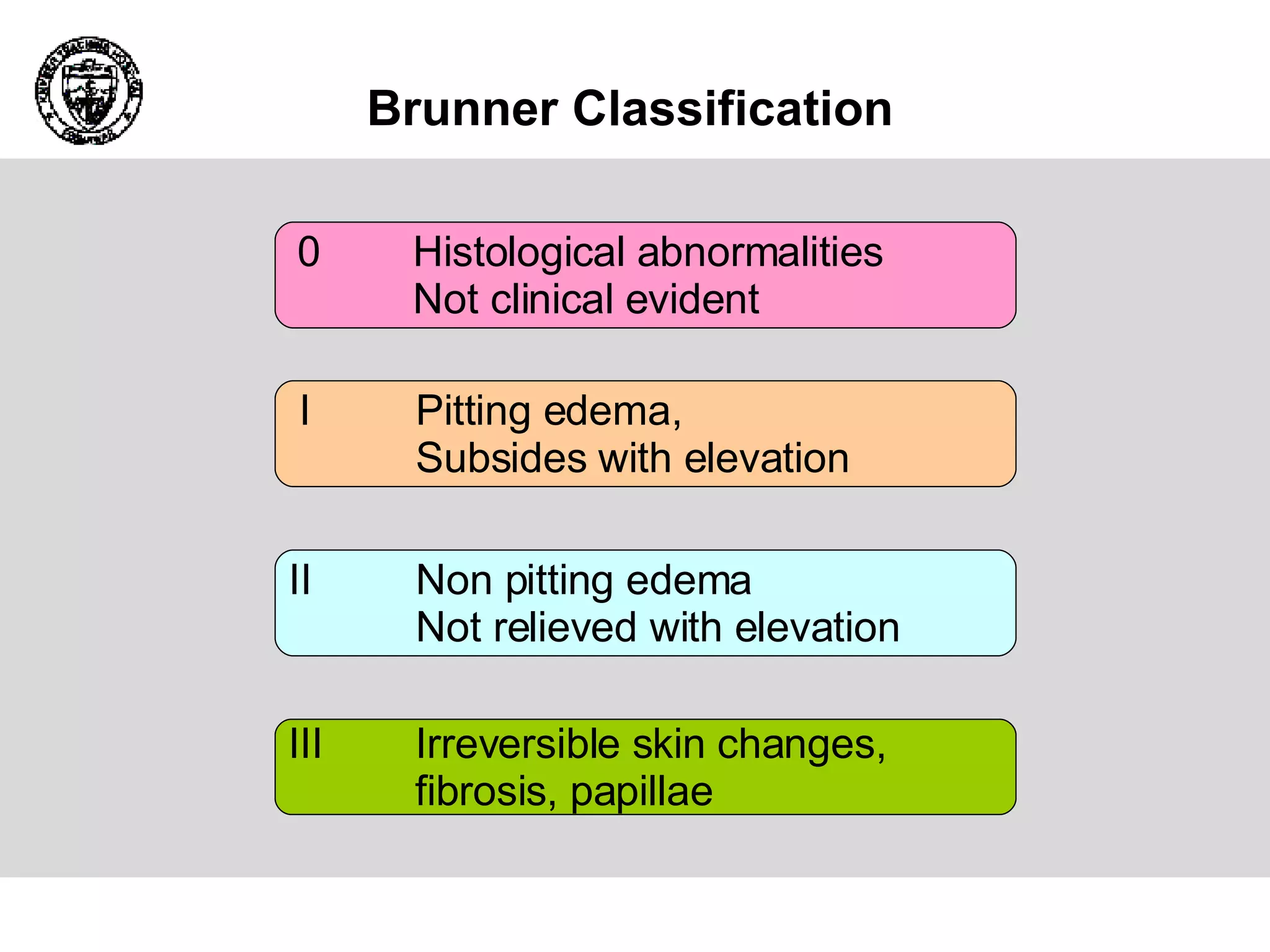
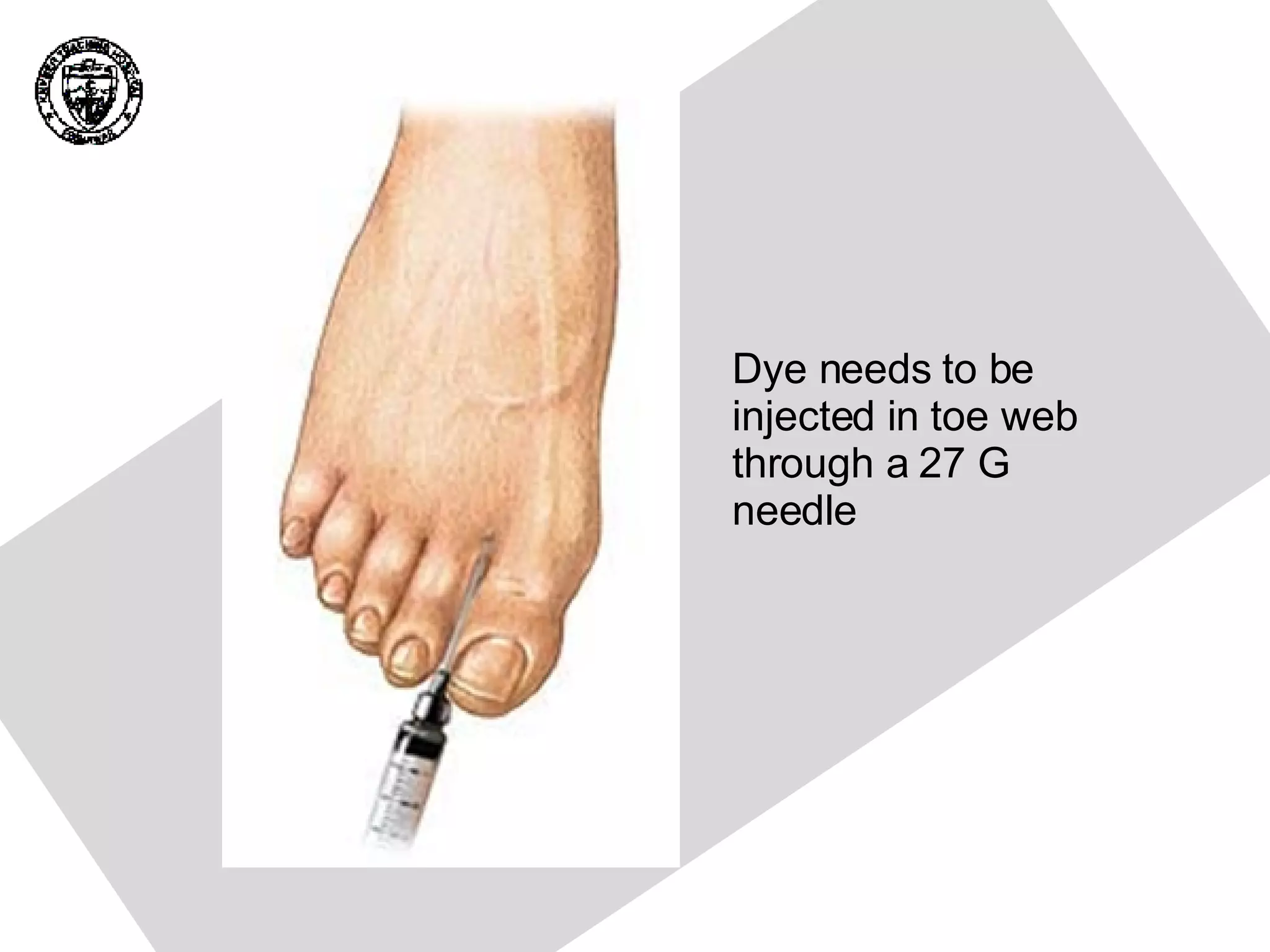
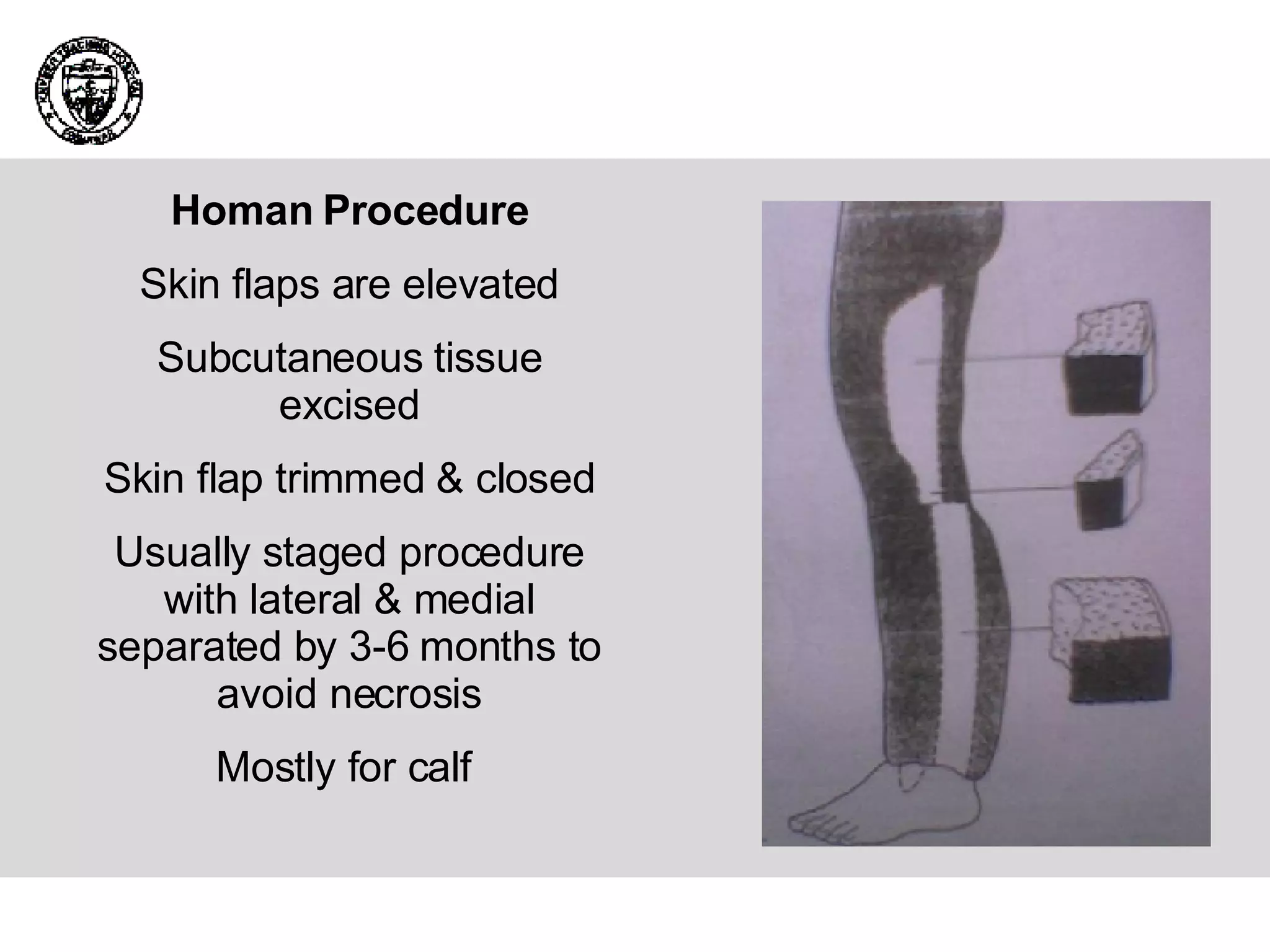
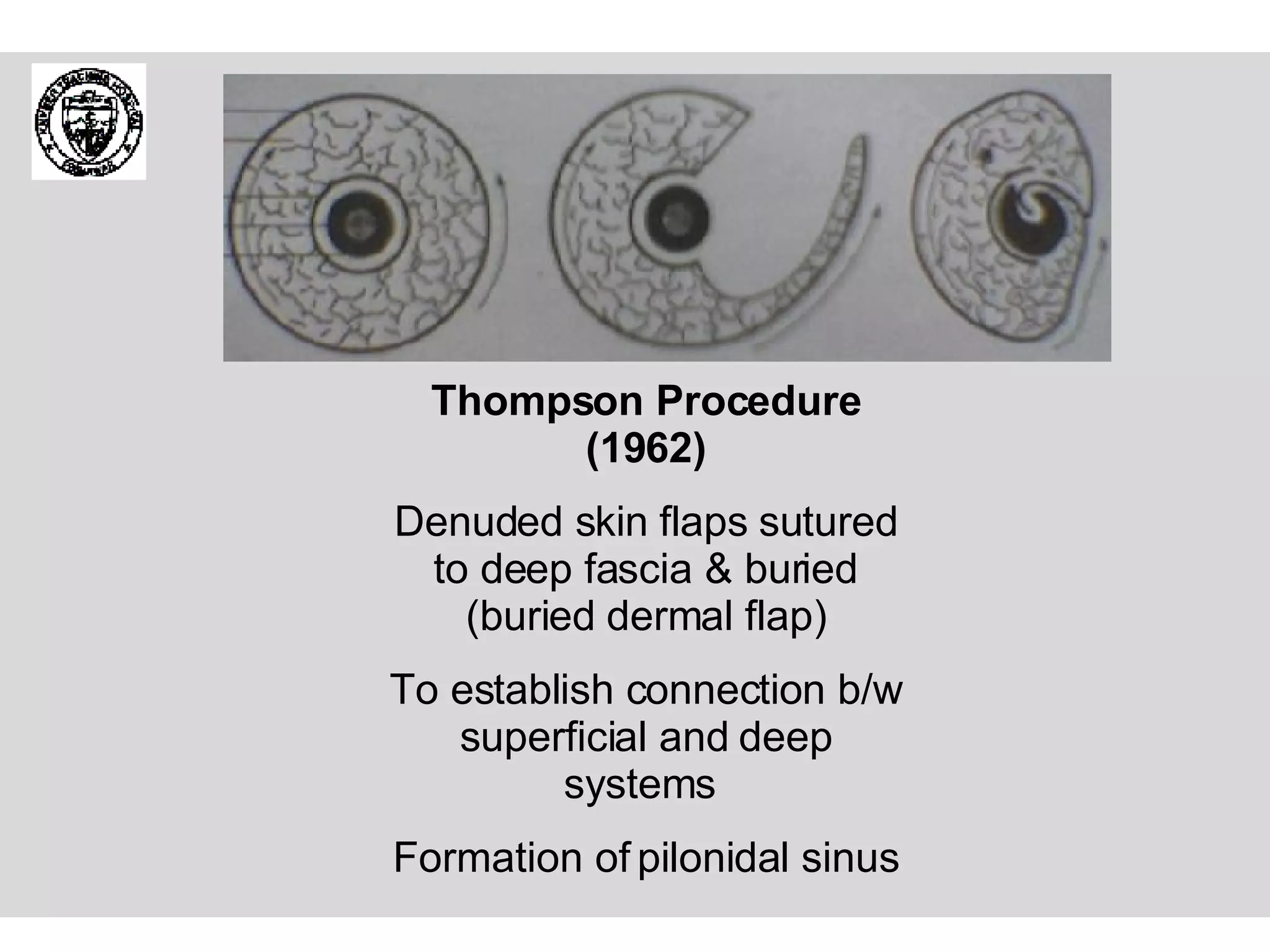
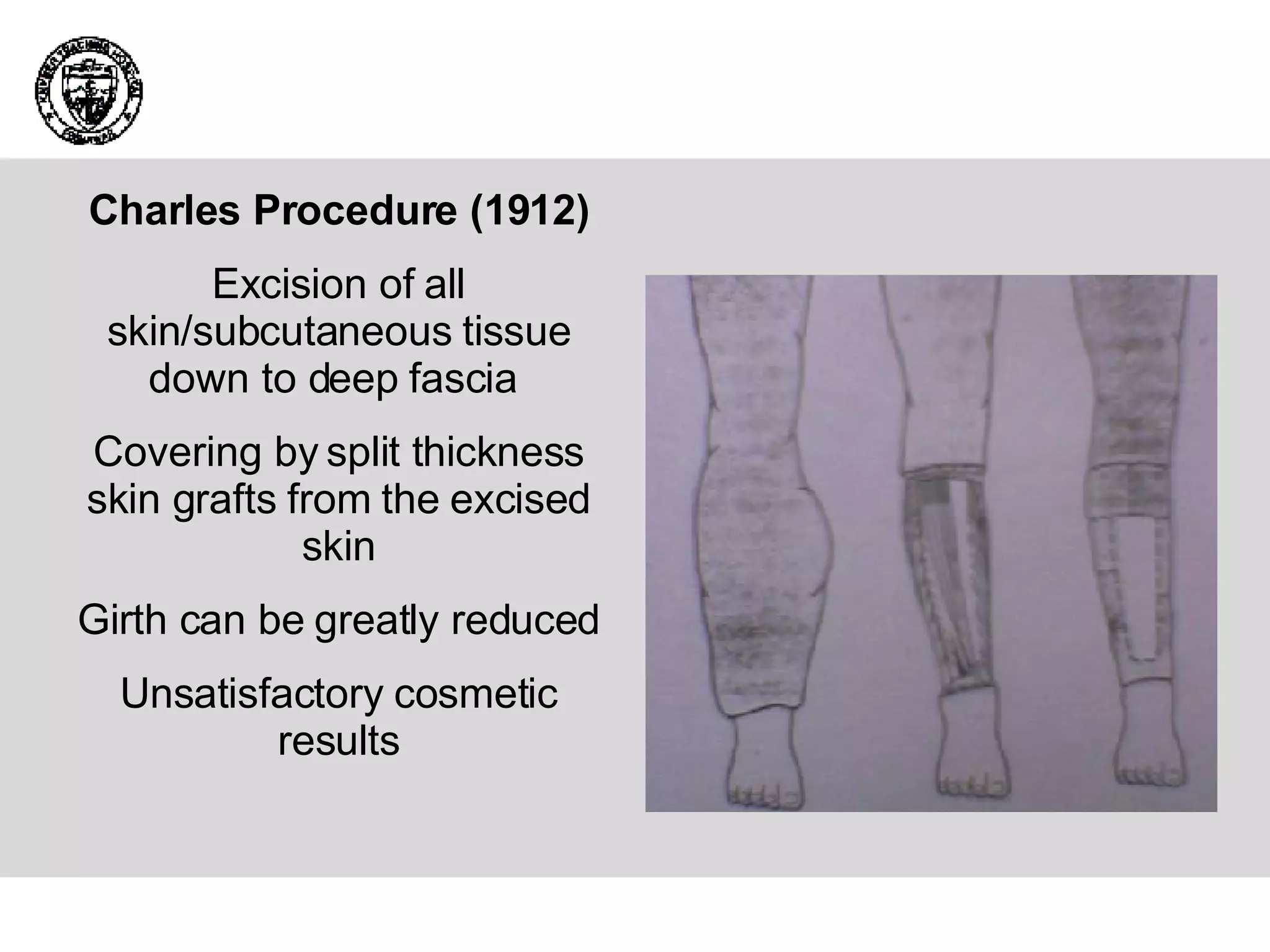
The document summarizes trends in lymphedema management. It discusses the basics of the lymphatic system, embryology, anatomy, pathophysiology, etiology of primary and secondary lymphedema, presentation, investigations, and treatment including conservative therapies like manual lymphatic drainage and compression garments as well as surgical procedures. Worldwide, it is estimated that 140-250 million people have lymphedema with filariasis being the most common cause.