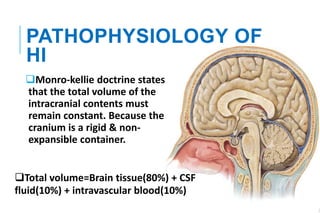
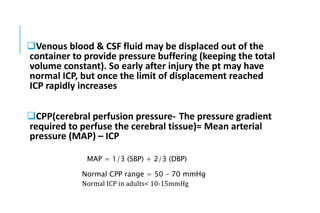
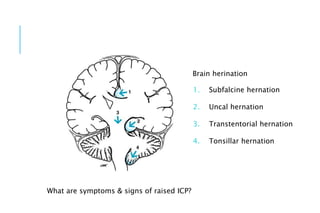
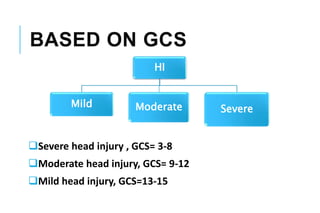
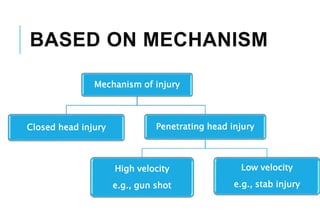
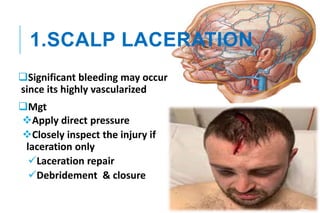
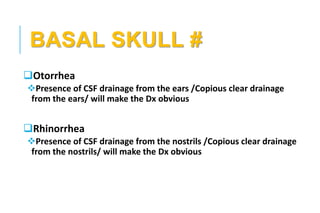
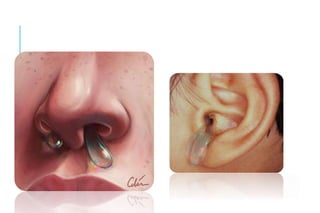
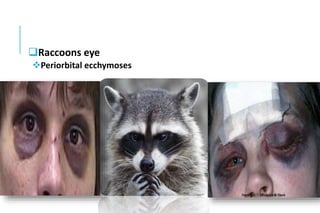
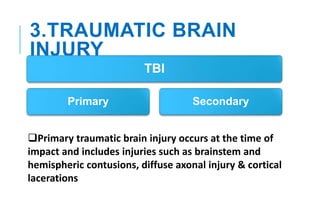
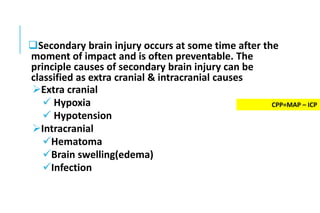
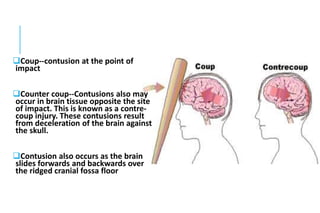
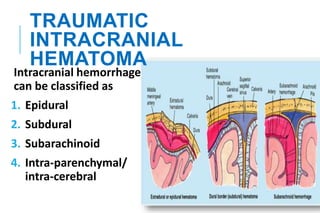
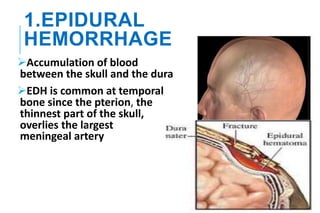
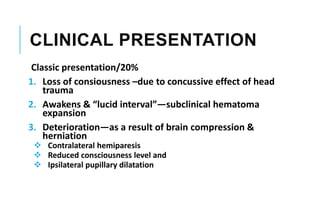
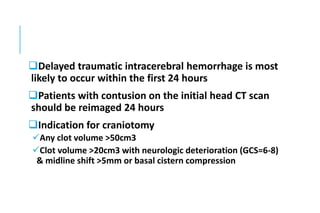
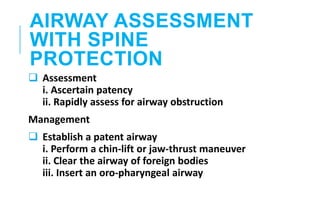
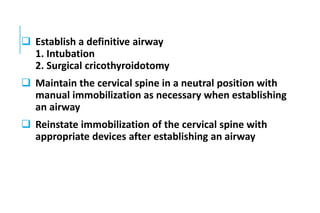
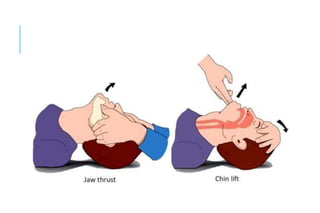
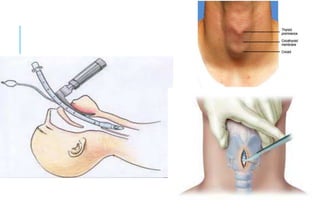
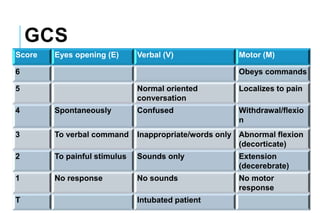
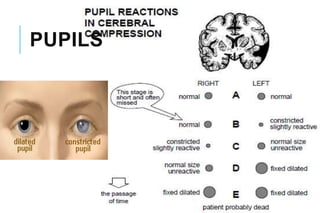
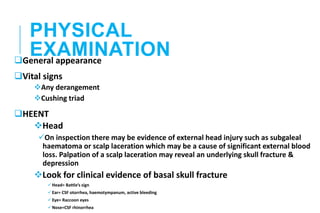
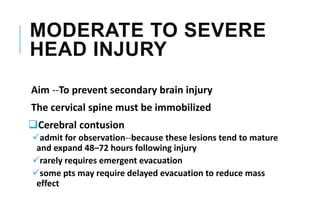
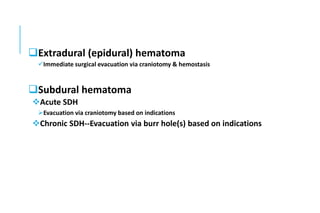
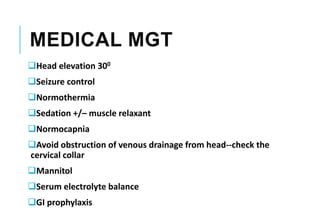
This document provides an outline on head injury (HI). It discusses the pathophysiology of HI, classification based on Glasgow Coma Scale and mechanism of injury. It describes the components of HI including scalp laceration, skull fractures, and traumatic brain injury. For traumatic brain injury, it covers concussion, contusion, diffuse axonal injury, and intracranial hematomas. It outlines the primary and secondary survey approach for patients with HI, including airway management, breathing, circulation, disability assessment, and exposure.