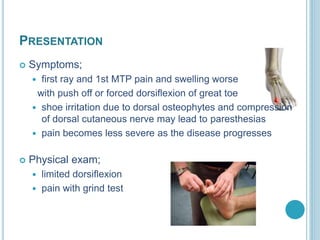
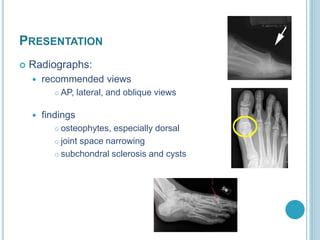
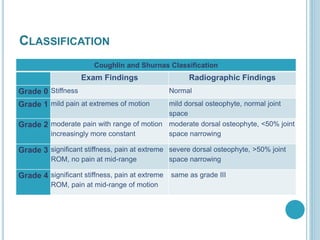
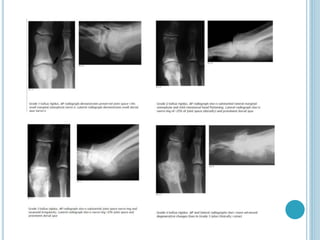
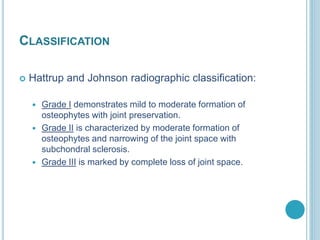
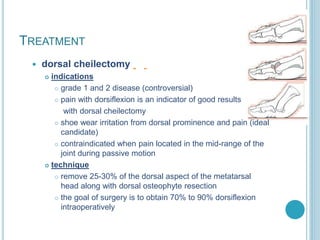
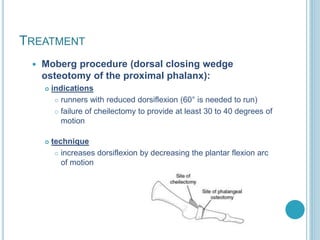
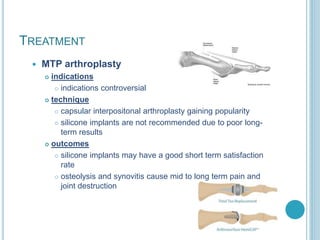
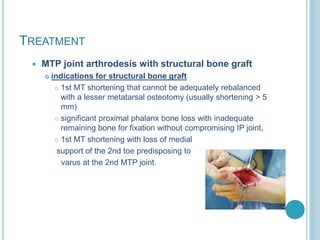
Hallux rigidus is a degenerative arthritis condition affecting the first metatarsophalangeal joint, leading to pain and limited motion, primarily in middle-aged females. Management options include non-operative treatments like NSAIDs and orthotics for early stages, while surgical options are available for advanced cases, including cheilectomy, arthroplasty, and arthrodesis. Classification systems aid in assessing the severity and treatment approach based on symptoms and radiographic findings.


![REFERENCES
• Coetzee J. C., Hurwitz S. R. , [ 2009] Arthritis & arthroplasty. The foot
and ankle , Saunders, an imprint of Elsevier Inc. , Philadelphia,
Pennsylvania, USA.
• Solomon L., Warwick D. , Nayagam S.,[2010] Apley’s System of
Orthopaedics and Fractures, 9th ed. Hodderarnold comp.,London, UK.
• Miller M. , Thompson S. , Hart J. ,[2012] REVIEW OF ORTHOPAEDICS
[PDF], 6th ed. by Saunders, an imprint of Elsevier Inc. , Philadelphia,
USA.
• Canale S. , Beaty J. , [2007] Campbell’s Operative Orthopaedics [PDF],
11th ed. By Mosby, An Imprint of Elsevier , Tennessee, USA.
• ORTHOPAEDIC REVIEW [2015] by orthobullets, [PDF], Collected By
Islam Gomaa Beltage.](https://image.slidesharecdn.com/halluxrigidus-161024151732/85/Hallux-rigidus-19-320.jpg)
