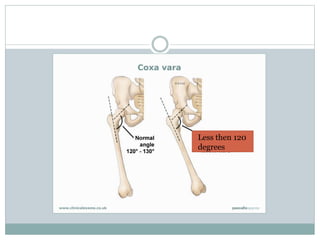
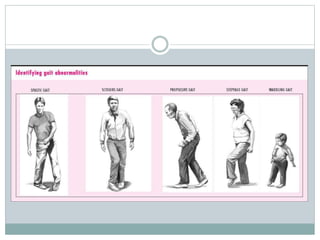
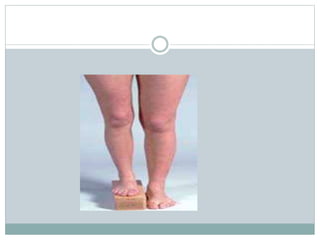
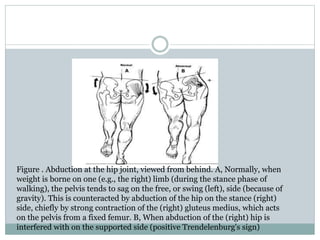
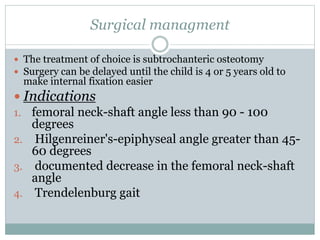
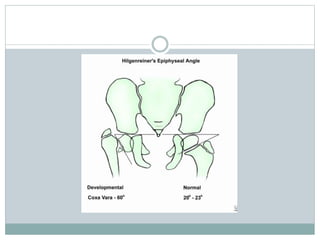
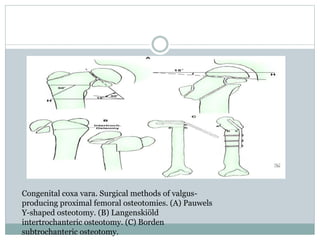
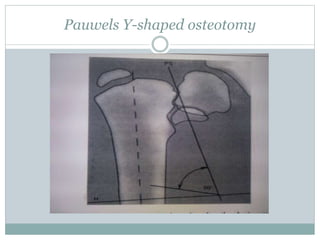
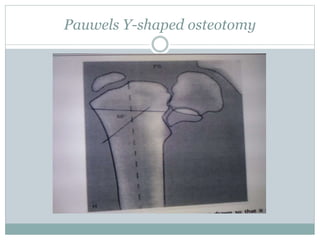
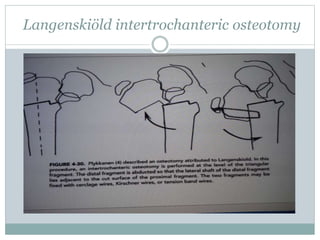
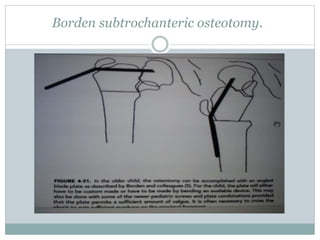
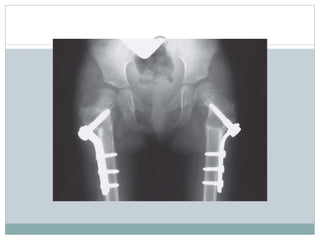
A 3-year-old girl presented with a limp in her right leg and was diagnosed with coxa vara. Coxa vara is a decrease in the angle between the femoral neck and shaft to less than 120 degrees. It can be congenital, developmental, or secondary to other bone diseases. Surgical management involves subtrochanteric osteotomy to correct the angle, which is fixed internally with plates or screws. Postoperative care includes casting for 8-12 weeks until radiographic healing is seen. Complications can include recurrence, physeal injury, or leg length discrepancy.