The document outlines a detailed guide for conducting a lower limb neurological examination, discussing the anatomy of the lumbar and sacral plexuses, their associated nerves, and their motor and sensory functions. It provides step-by-step instructions on conducting various assessments, including gait, tone, power, reflexes, sensation, and coordination. The examination aims to evaluate neurological health in patients by identifying signs of upper or lower motor neuron lesions and sensory abnormalities.
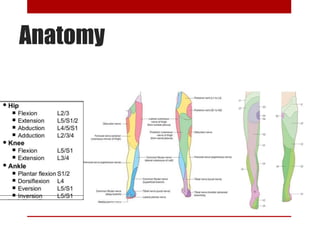
![Anatomy
• Lumber plexus:
formed by the anterior rami (divisions) of the
lumbar spinal nerves L1, L2, L3 and L4. It also
receives contributions from thoracic spinal nerve
12. These roots divide into several cords. These
cords then combine together to form the six major
peripheral nerves:
1. Iliohypogastric Nerve [(L1 (with contributions
from T12)]
Motor: Innervates the internal oblique and
transversus abdominis.
Sensory: Innervates the posterolateral gluteal skin in
the pubic region.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-2-320.jpg)
![Anatomy
2. Ilioinguinal Nerve [L1]
Motor: Innervates the internal oblique and
transversus abdominis.
Sensory: skin on the upper middle thigh In males,
it also supplies the skin over the root of the penis
and anterior scrotum. In females, it supplies the
skin over mons pubis and labia majora.
3. Genitofemoral Nerve [L1, L2]
Motor: cremasteric muscle.
Sensory: The genital branch innervates the skin of
the anterior scrotum (in males) or the skin over
mons pubis and labia majora (in females). The
femoral branch innervates the skin on the upper
anterior thigh.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-3-320.jpg)
![Anatomy
4. Lateral Cutaneous Nerve of the Thigh
[L2,L3]
Motor: None
Sensory: anterior and lateral thigh down to
the level of the knee.
5. Obturator Nerve [L2, L3,L4]
Motor: obturator externus, pectineus, adductor
longus, adductor brevis, adductor magnus,
gracilis.
Sensory: Innervates the skin over the medial
thigh.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-4-320.jpg)
![Anatomy
6. Femoral Nerve [L2,L3,L4]
Motor: Illiacus, pectineus, sartorius, all the
muscles of quadriceps femoris.
Sensory: skin on the anterior thigh and the medial
leg as a saphenous nerve.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-5-320.jpg)
![Anatomy
• Sacral plexus:
formed by the anterior rami (divisions) of the sacral
spinal nerves S1, S2, S3 and S4. It also receives
contributions from the lumbar spinal nerves L4 and L5.
these spinal roots (and the lumbosacral trunk) divide into
several cords. These cords then combine together to form
the five major peripheral nerves:
1. superior gluteal nerve [L4, L5, S1]
Motor: gluteus minimus, gluteus medius and tensor
fascia lata
Sensory: None](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-6-320.jpg)
![Anatomy
2. Inferior gluteal nerve[ L5, S1, S2]
Motor: Innervates gluteus maximus
Sensory: none.
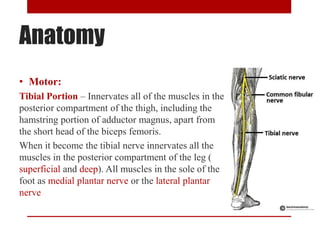
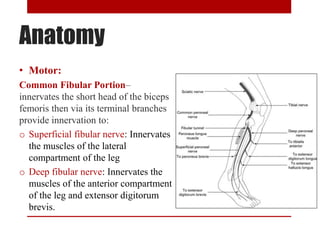
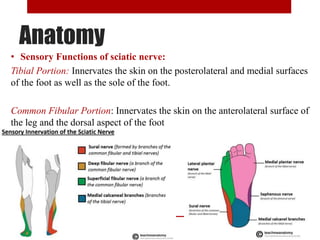
3. Sciatic Nerve [L4, L5, S1, S2, S3]
derived from the lumbosacral plexus.
When the sciatic nerve reaches the apex of
he popliteal fossa, it terminates by
bifurcating into the tibial and common
fibular nerves.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-7-320.jpg)
![Anatomy
4. Posterior Femoral Cutaneous: [S1, S2, S3}
Motor : none
Sensory : skin on the posterior surface of the thigh
and leg and skin of the perineum.
5. Pudendal Nerve: [S2, S3, S4]
Motor: skeletal muscles in the perineum, the external
urethral sphincter, the external anal sphincter, levator
ani.
Sensory: penis and the clitoris and most of the skin
of the perineum.](https://image.slidesharecdn.com/lowerlimbneurologicalexamination-161215100110/85/Lower-limb-neurological-examination-11-320.jpg)