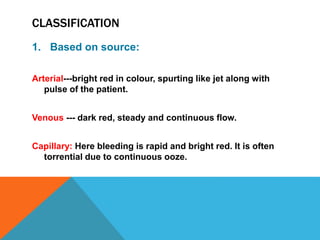
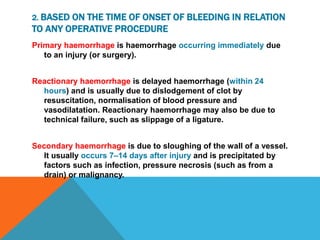
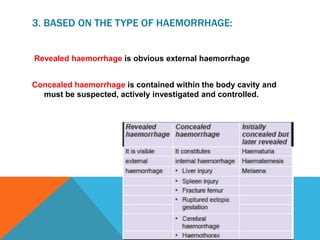
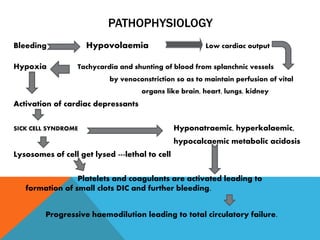
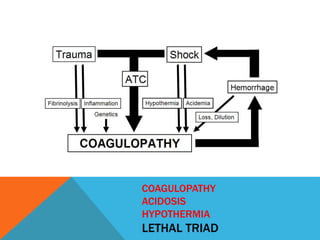
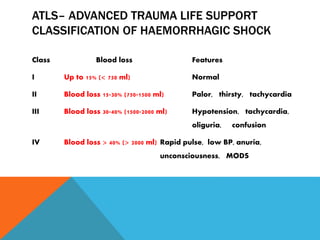
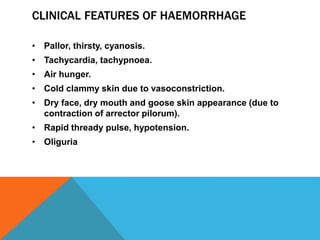
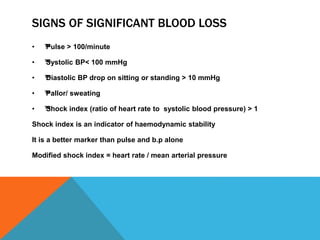
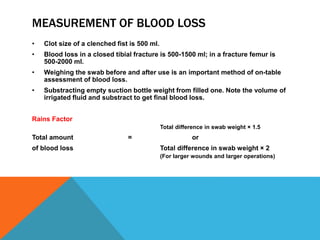
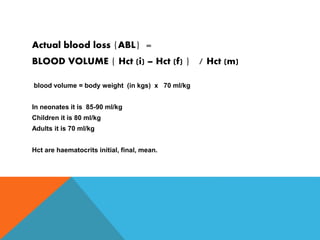
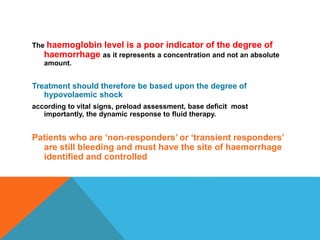
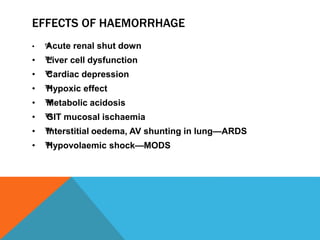
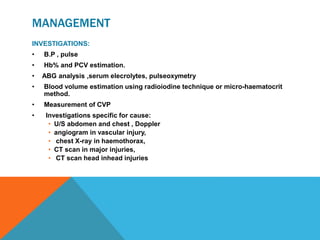
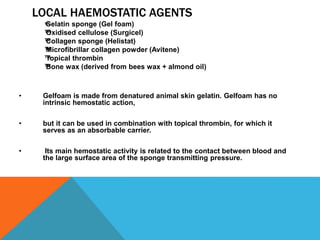
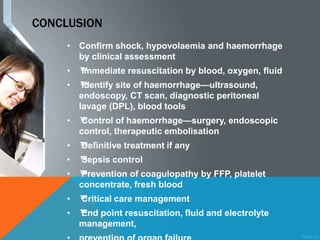
This document discusses the classification, pathophysiology, clinical features, and management of haemorrhage. It classifies haemorrhage based on source, time of onset, type, duration, and possible intervention. Management involves identifying and controlling the bleeding through resuscitation, investigating the bleeding site, achieving haemorrhage control through surgery or other techniques, and practicing damage control resuscitation to prevent physiological exhaustion. Local haemostatic agents, fluid resuscitation, blood transfusion, and sepsis control are also important in managing haemorrhage.