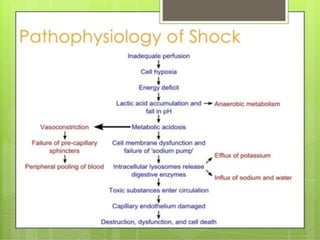
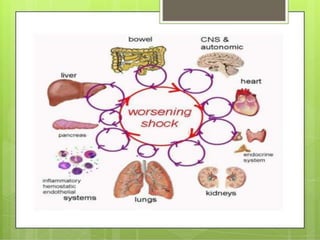
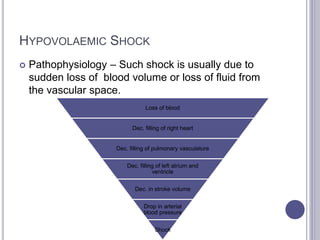
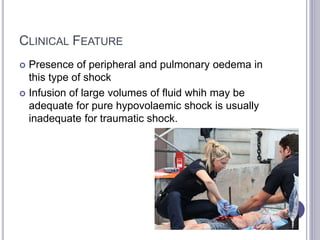
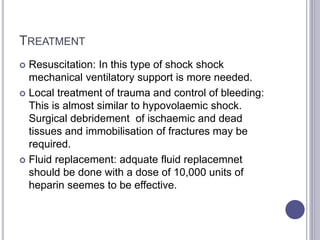
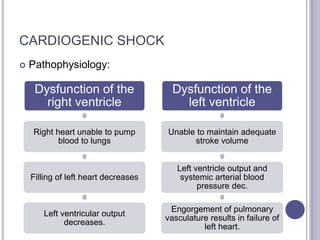
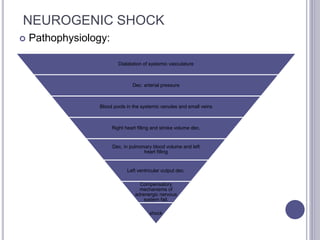
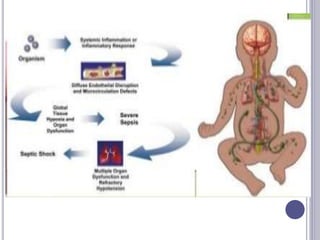
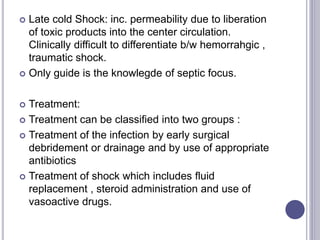
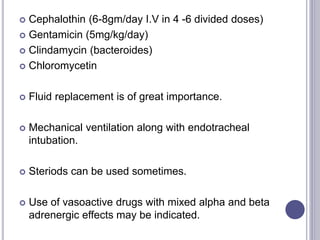
This seminar covers different types of shock including definitions, pathophysiology, clinical features, investigations, and treatment. The main types discussed are hypovolaemic shock, traumatic shock, cardiogenic shock, neurogenic shock, septic shock, and crush syndrome. Hypovolaemic shock is the most common and results from sudden loss of blood or fluid volume. Treatment focuses on fluid resuscitation and controlling bleeding. Septic shock has a high mortality and is usually caused by gram-negative bacteria. Crush syndrome occurs after body portions are compressed by heavy weights.