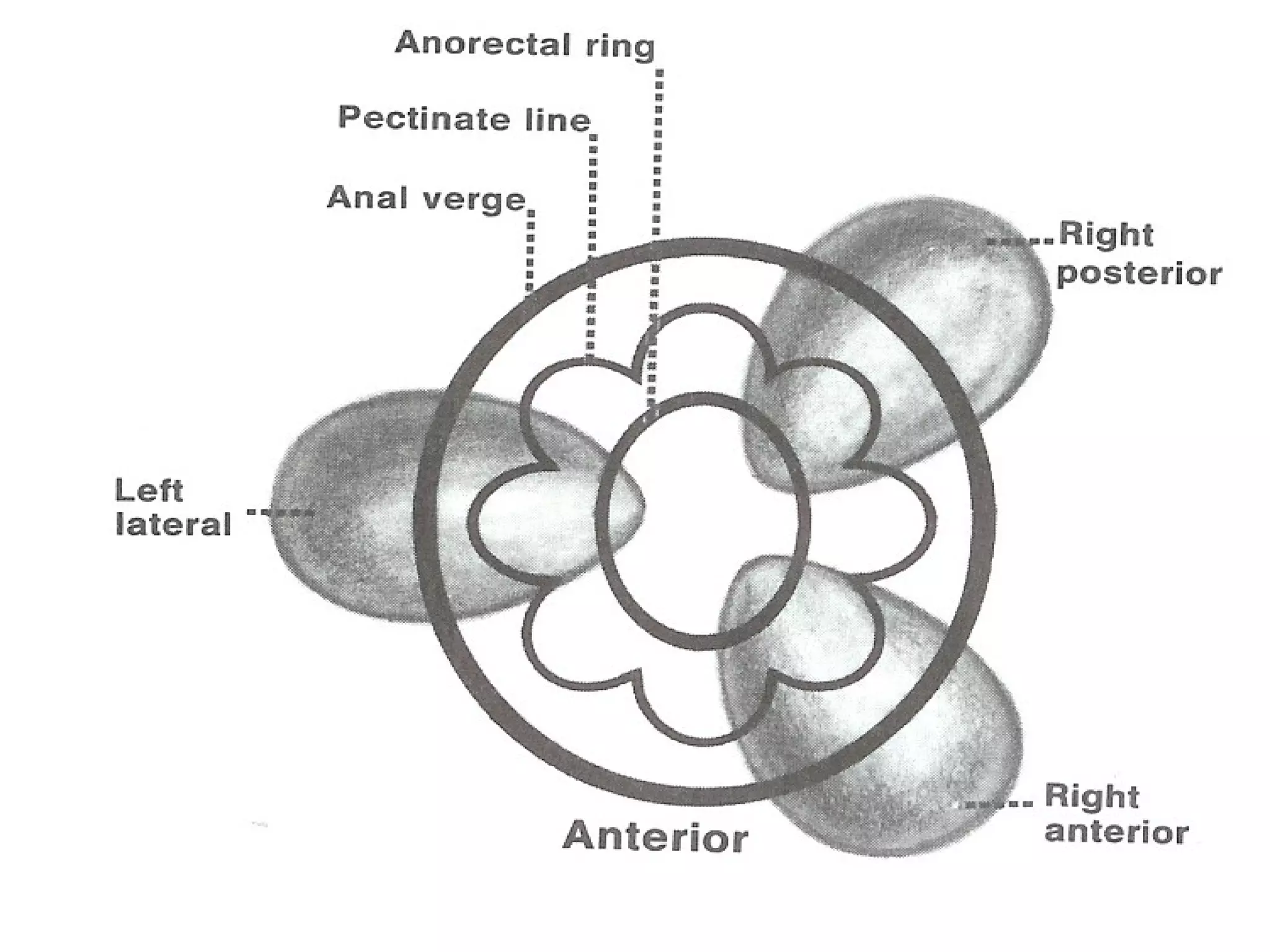
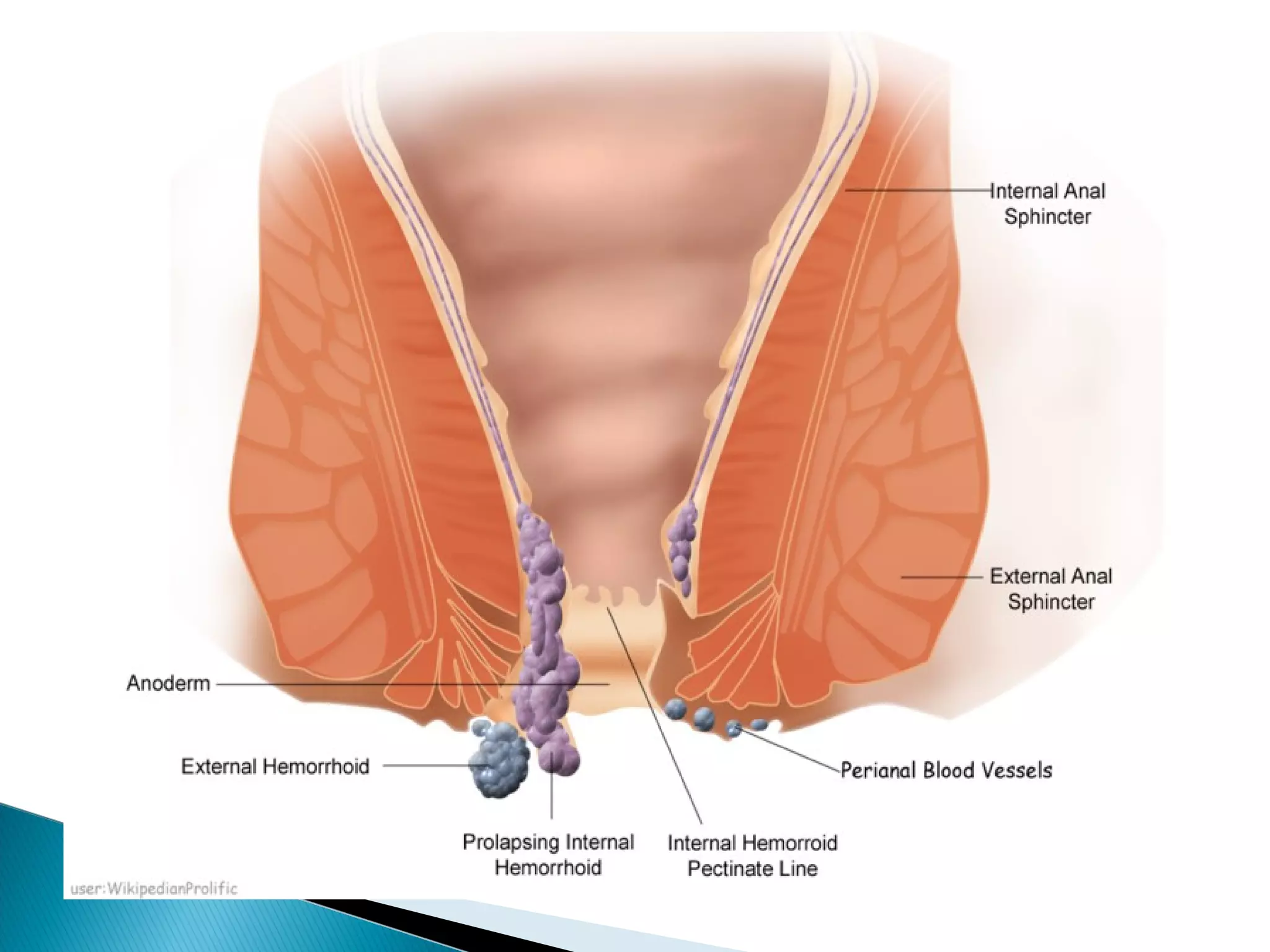
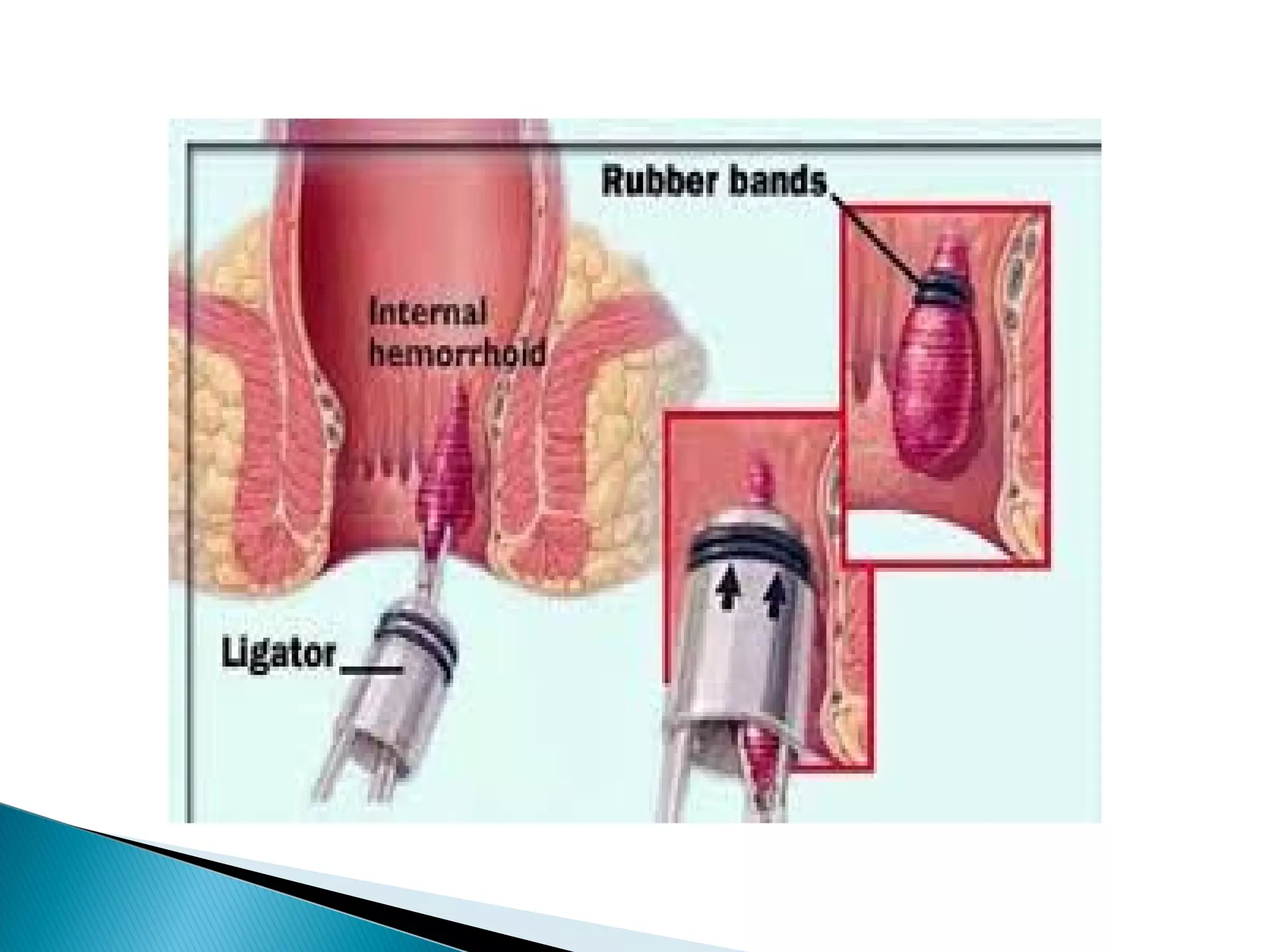
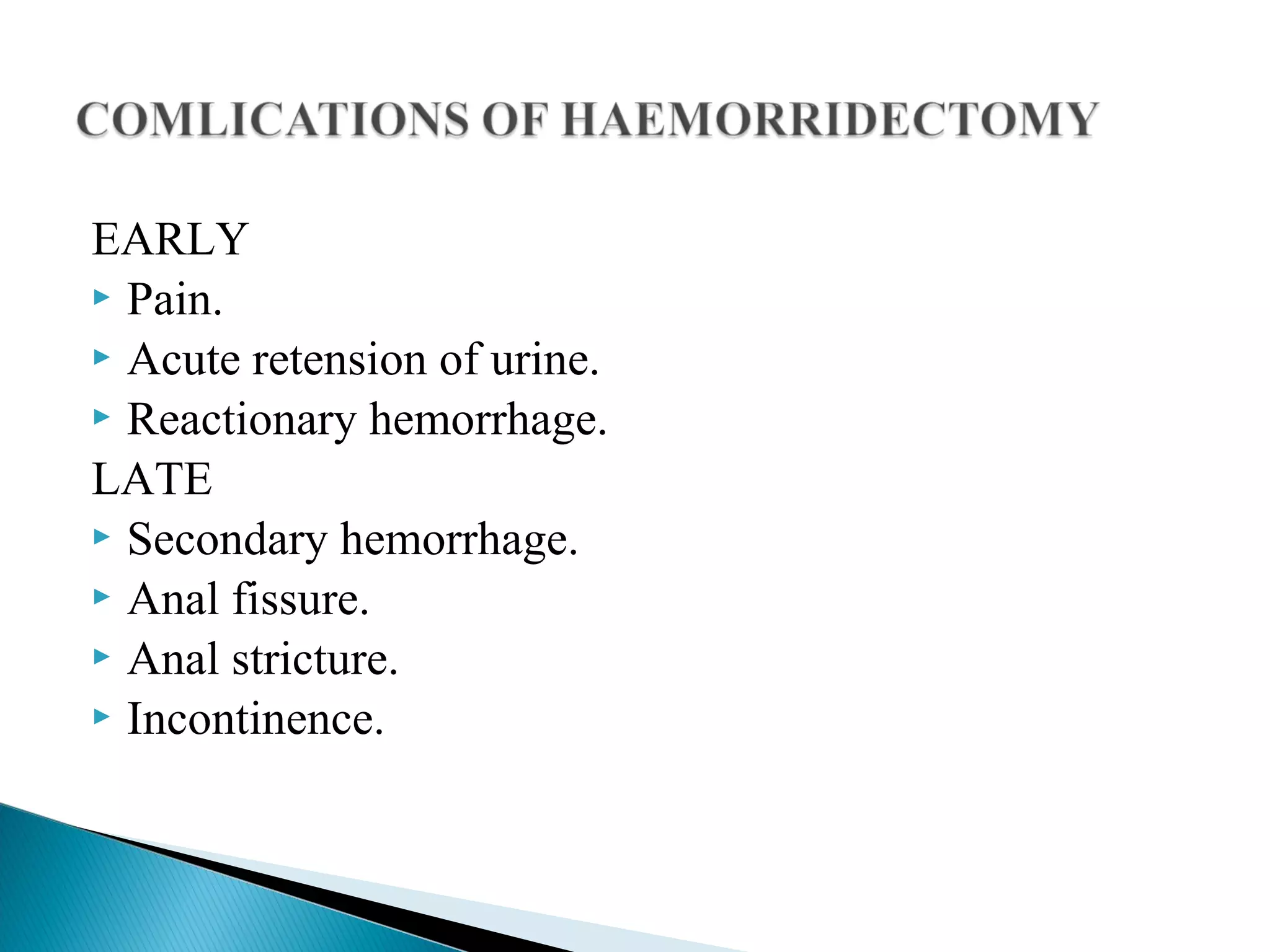
Haemorrhoids are normal anal cushions that can become symptomatic due to straining, constipation, pregnancy, obesity and other factors. They are classified based on their location relative to the dentate line. Conservative treatments are recommended for grade I/II haemorrhoids while more severe or symptomatic cases may require non-surgical procedures like rubber band ligation or surgical haemorrhoidectomy. Potential complications depend on the severity but can include pain, bleeding and infection. Differential diagnosis includes other anorectal conditions.