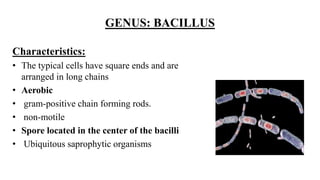
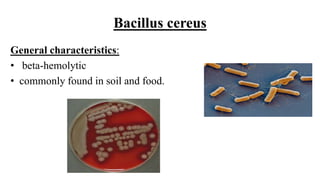
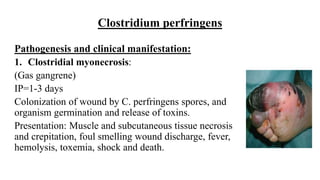
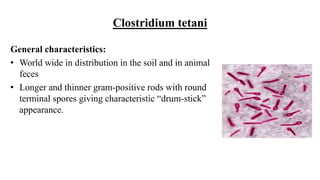
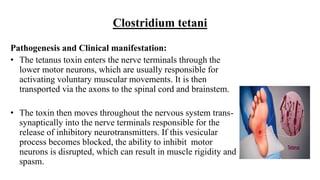
Scientists divide Gram-positive bacilli into spore-forming and non-spore-forming genera. The two spore-forming genera are Bacillus and Clostridium. Bacillus forms endospores centrally and is aerobic. Important pathogenic Bacillus species include B. anthracis and B. cereus. B. anthracis causes anthrax through its toxin and spores. Clostridium forms terminal or subterminal spores and is anaerobic. Important pathogenic Clostridium species are C. perfringens, C. tetani, and C. botulinum, which cause myonecrosis, tetanus, and botulism respectively through their tox